NL Journal of Dentistry and Oral Sciences
(ISSN: 3049-1053)
The Challenge of Retrofitting A Survey Crown to an Existing Partial Denture
Author(s) : Guilherme A Arossi, Kelsey Renn, Adam Eisner, Qoot Alkhubaizi. DOI : 10.71168/NDO.02.03.120
Abstract
Background: The long-term success of removable partial dentures, in part, relies on preservation of the abutment teeth and patient adaptation. Objective: This paper aims to describe the maintenance of contours and retentive preparations on abutment teeth while retrofitting crowns to existing removable partial denture, using Lithium-Dissilicate milled crowns. Clinical Considerations: This case report describes a practical and innovative approach to preserve restorable removable partial denture prosthesis abutment teeth using a digital workflow. This method utilizes the feature of “biogeneric copy” in the scanner software replicating the preparation features and contours of 4 abutment teeth. Four lithium disilicate indirect restorations were designed, fabricated and milled in-house and delivered on the same day. Based on clinical and patient evaluations, the denture insertion and retention were maintained and comparable to its original status. Conclusion: This technique is a viable alternative to the standard analogue technique that could potentially introduce inaccuracies and delays in treatment. With modern technological advances, it has become necessary to archive digital images of RPD abutment teeth anatomy for future utilization of restorative treatment. Keywords: CAD-CAM; Removable Partial Denture; lithium disilicate; retrofit surveyed crown; abutment teeth; same-day crown.
Introduction
Using removable partial dentures (RPD) enhances the oral health of edentulous patients by replacing multiple missing teeth [1]. RPD design requires retention features, insertion axis guide planes, and rest areas on abutment teeth. These features can either be on natural dentition or lab-fabricated full coverage crowns called survey crowns. They provide support, stability, assist with proper seating and allow occlusal forces distribution [2]. During planning for the RPD, the dentist determines the need for different restorative treatments for abutment tooth based upon their clinical conditions.
Caries and cuspal fractures frequently compromise abutment teeth [2,3,4]. Modifying RPD abutment teeth and the existing RPD requires compliance and a risk vs benefits analysis. When patients have a functional RPD, they will prefer to keep it, repairing only the damaged abutment teeth [2,3,5]. The fabrication of a survey crown to retrofit within an existing RPD is technically challenging chairside [4,6].
Several methods for retrofitting a survey crown to an existing RPD were described [7]. The use of acrylic pattern adapted to both preparation and RPD allows the lab technician to produce such crown [5]. This approach is time-consuming for the dentist and the patient must endure long appointments [8,9]. Alternatively, taking two impressions, one to produce the working model and another with the RPD to guide the lab adjustments. With this technique the patient must accept being without their RPD while the lab fabricates the survey crown [6,9]. The overriding concern is how a dentist communicates the configuration of the rest seat(s), retentive clasps, and reciprocal elements to the laboratory technician [10].
CAD/CAM technology allows the fabrication of an all-ceramic survey crown to be retrofitted to an existing RPD [6]. The accuracy of the scan affords a precise duplication of the pre-existing crown feature [1]. Additionally, the patient does not have to be without their prosthesis [6]. This procedure offers the patient an alternative to the fabrication of a new survey crown without the need for a new RPD [1].
Retrofitting survey crowns utilizing digital workflow may require different CAD/CAM techniques. When abutment teeth are completely damaged, one must scan the prepared teeth, the opposing arch, occlusal relationship, and the existing RPD in situ. Scanned files may be indexed in a design software, and the survey crown would be designed and manufactured [8]. When the abutment tooth maintains its RPD design features, the Cerec® utilizes a CAD mode known as “Biogeneric Copy” replicating preexisting size, shape, and form of the abutment tooth enabling chair-side fabrication of survey crown [1].
This case report is describing a clinical scenario where abutment teeth of a well-fitting RPD prosthesis were treated restoratively with minimal impact to the denture fit.
Case Report
A 67-year-old female patient presented to the clinic as an irregular attender and was open to any recommended treatment. She was seeking episodic care with no specific chief complaints and had limited finances. The patient had a RPD which she was satisfied with. Medically, she was ASA II [11], and none of her medications or allergies impacted her dental management (Figure 1).
 Figure 1: Initial picture of patient’s smile.
Figure 1: Initial picture of patient’s smile.
Extra-oral examinations revealed crepitus in the temporomandibular joint. Patient reported no pain in the area or limitation to range of motion. Intra-orally, all soft- and residual hard-tissues were within normal limits. The patient is a Kennedy class III [12] at sites of teeth number #3, #7, #8, and #13. The RPD was well designed and adapted to the rest seats of teeth number #2, #4, #12 and #14 (Figure 2 and 3). A full mouth radiograph series was taken, and a comprehensive clinical evaluation was performed. The patient’s periodontal diagnosis was Stage IV, Grade A periodontitis [14]. Clinical findings evidenced defective restorations as well as caries on teeth number #2, #4, #5, #12, #18, #19, #10 and #20 (Table 1).
 Figure 2: Occlusal pictures of patient’s initial condition without RPD.
Figure 2: Occlusal pictures of patient’s initial condition without RPD.
 Figure 3: Occlusal pictures of patient’s initial condition with RPD.
Figure 3: Occlusal pictures of patient’s initial condition with RPD.
Upon completion of diagnostics, a treatment plan was formulated addressing patient’s needs and expectations. All diagnostic information, proposed treatment, benefits, and risks were presented, and an informed consent was signed. The retentive capacity of the partial denture abutment teeth was not impaired by the presence of caries and defective restorations. We aimed to restore the abutment teeth while preserving their design features maintaining the functionality of the RPD. The treatment planning included biogeneric copy CAD/CAM crowns in teeth number #4, #5, #12, #19, biogeneric copy CAD/CAM Inlay/Onlay in teeth number #2 and #18; and direct resin-based composite restorations in teeth number #10, #20, #28 and #29 (Table 1).
| Tooth | Findings | Treatment plan |
| 2 | Mesio-occlusal rest seat, root caries, defective resto- ration | biogeneric copy Lithium Disilicate (LD) Inlay (CEREC) |
| 4 | Disto-occlusal rest seat, caries, defective restoration. | biogeneric copy LD ¾ crown |
| 5 | Root caries, defective restoration | biogeneric copy LD ¾ crown |
| 6 | Porcelain chipping, buccal defective crown margin | Resin Modified Glass Ionomer cement to seal margins |
| 10 | Disto-lingual caries | DL direct composite restoration |
| 12 | Disto-occlusal rest seat, caries, defective restoration | biogeneric copy LD crown |
| 18 | Fractured disto-mesial restoration | Mesial-Occlusal-Buccal-Lingual onlay |
| 19 | Mesial caries, furcation involvement, defective restoration | core build up, full coverage crown |
| 20 | Disto-occlusal caries | Disto-Occlusal direct composite restoration |
| 28; 29 | Buccal abfraction | direct composite restorations |
Table 1. Clinical findings and treatment planning.
Photographs (Nikon Inc, Melville, NY) and intraoral scan (OmniCam CEREC Dentsply/Sirona, Charlotte, NC) of both arches were taken. Restorations were removed from teeth number #2, #4, #5 and #12 using a round diamond and 245-carbide burs (Komet USA, Rock Hill, SC). Selective caries removal was completed using low- speed ceramic bur (CeraBur, Komet USA, Rock Hill, SC), under rubber dam isolation. Immediate dentin sealing was achieved using universal adhesive (Prime&Bond Elect; Dentsply Caulk, York, PA), followed by placement of a thin layer of resin-based composite (TPH Spectra; Dentsply Caulk, York, PA) to block undercuts in the preparation.
Preparations were completed using a rounded-end tapered diamond bur (Komet USA, Rock Hill, SC). Minimally invasive preparations of teeth number #2, #4 and #5 (Figure 4) allowed the preservation of sound tooth structure on the lingual area of the premolars and both buccal and lingual cusps of the molar. Tooth number #12 was planned for a full coverage restoration. Once finished, a retraction cord (Ultrapak; Ultradent, South Jordan, UT) was placed intrasulcular around each preparation.
 Figure 4: Digital model of the preparations of teeth #2, #4, #5
Figure 4: Digital model of the preparations of teeth #2, #4, #5
A scan of the prepared teeth was taken, and the restorations were digitally designed using the preoperative scan data, mimicking each tooth contour prior to the preparation (Figure 5). When all CADs were completed, the restorations were milled out of LD ceramic blocks (E-max, Ivoclar/Vivadent, Somerset, NJ) using a milling machine (MCXL; Dentsply/Sirona, Charlotte, NC).
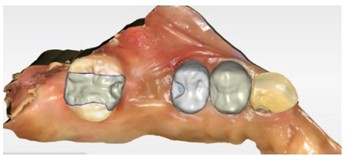 Figure 5: CAD CEREC’s ” biogeneric copy“ of the initial abutment teeth morphology.
Figure 5: CAD CEREC’s ” biogeneric copy“ of the initial abutment teeth morphology.
The blue-phase e-max onlays had the sprues removed and were tried into the patient’s mouth (Figure 6). After verifying all clinical and radiographic adaptations, the patient’s RPD was seated to ensure the onlays and crowns were retrofitting properly (Figure 7). The blue-phased e-max were polished (Dialite LD; Brasseler, Savannah, GA) and fired at the oven (Programat CS, Ivoclar/Vivadent, Somerset, NJ) following the manufactures’ recommendations.
 Figure 6: Intra-oral fitting check of Inlay (#2) and partial crown (#4, #5) of LD in purple stage.
Figure 6: Intra-oral fitting check of Inlay (#2) and partial crown (#4, #5) of LD in purple stage.
 Figure 7: RPD clinical seating assessment over purple stage LD crowns.
Figure 7: RPD clinical seating assessment over purple stage LD crowns.
The completed onlays and crowns were cemented using resin-based adhesive cement. The intaglio surface of each restoration was etched for 20 seconds using hydrofluoric acid (Ultradent, South Jordan, UT), rinsed and dried. Monobond plus (Ivoclar/Vivadent, Somerset, NJ) was used as ceramic primer. The enamel of all preparations was etched with 37% phosphoric acid (Dentsply/Sirona, Charlotte, NC) for 30 seconds, rinsed and dried. Universal adhesive (“Adhese” Ivoclar/Vivadent, Somerset, NJ) was actively applied to all surfaces, air thinned, and light cured with a 1,470 mW/cm2 light curing unit (Paradigm DeepCure, 3M Oral Care, St. Paul, MN). Each restoration was cemented separately. Dual-cure resin-based cement (Variolink; Ivoclar/Vivadent, Somerset, NJ) was placed on the intaglio surface, seated in position, and light-cured for 3 seconds. Excess was removed, followed by 40 seconds of light curing exposure. After cementation, the patient was able to try in the RPD, and minor adjustments were made to occlusal contacts and seating, using a fine-grit diamond bur (Figures 8, 9 and 10). All adjusted areas were polished (Brasseler, Savannah, GA).
 Figure 8: Occlusal view pictures of patient’s final condition without RPD.
Figure 8: Occlusal view pictures of patient’s final condition without RPD.
 Figure 9: Occlusal view pictures of patient’s final condition with RPD.
Figure 9: Occlusal view pictures of patient’s final condition with RPD.
 Figure 10: Final picture of patient’s smile after treatment was finished.
Figure 10: Final picture of patient’s smile after treatment was finished.
Discussion
Retrofitting a surveyed crown to an existing RPD is challenging [10]. Traditional methods may result in capture discrepancy of the RPD orientation to the abutment features impacting seating at the guiding planes [1,10]. The digital process expedites the procedure by eliminating the need for analogue impressions [6], the distortions during the crown’s manufacturing steps and the prolonged appointments destined for clinical adjustments [1,6,9].
Patients using RPD are dependent on the prosthesis and are unable to part with it while being retrofitted in the laboratory [1,3,6]. The clinical chair-side technique described in this case report allows for better patient acceptance. This method is well suited when the design features of the abutment tooth have acceptable clinical parameters [1,3]. This approach allows faster treatment completion without the need of a dental laboratory [1]. The biogeneric copy mode allows a same day result providing reproduction of preoperatory conditions with minimal need for intra-oral adjustments [9,10]. The digital approach is advantageous to the dentist and patient. Scans files can be easily stored for later use and laboratory expenses minimized. Additionally, the dentist can correct defective preparation margins after analysis of the digital impression, or the restoration’s shade during glazing procedures, if they are below acceptable levels [3,4]. Nevertheless, the dentist will dedicate many working hours to care of one case, significantly impacting daily production, and incurring a large patient fee. For patients, spending long appointments at the dental office can be daunting. If the patient or dentist cannot commit to lengthy appointments, a traditional PVS impression and scan of the stone models can produce a CAD/ CAM retrofitted crown [4,5]. This technique reduces clinical time; however, it may produce dimensional errors [8]. The digital workflow demands expensive equipment. Other than intra-oral scanners, the dentist must acquire a milling machine and a firing oven, both costly equipment that demands training with a long learning curve to competently use them [15].
Full metal or porcelain fused to metal crowns are the restoration of choice for survey crowns [3,4]. Nowadays, dentists might use zirconia crowns, however, when retrofitting is needed, both options require lab time. LD restorations present an option for a fast-paced workflow, maintaining the strength required for such a challenge, especially for a tooth-supported RPD [1]. Moreover, LD provides a high adhesive cementation bond producing a flexural strength ranging from 360 to 400 MPa [1], allowing the manufacturing of partial non-retentive crowns.
Conclusion
In conclusion, retrofitting a crown under an existing RPD using chairside CEREC CAD/CAM technology has been shown to be predictable, accurate, durable, and esthetic [2,10]. Biogeneric copy mode can be used if original tooth structure provides an adequate fit for RPD [1,2]. Patient satisfaction is enhanced due to speed, aesthetics, and functionality of CAD/CAM fabrication.
References
1. Patel D. Retrofitting a Crown Supporting a Removable Partial Denture Using “Biogeneric Copy” to Replicate Tooth’s Preoperative Condition. Compend Contin Educ Dent. 2016;37(2):126-130.
2. Ozawa D, Suzuki Y, Kawamura N, Ohkubo C. Fabrication of crown restoration retrofitting to existing clasps using CAD/CAM: fitness accuracy and retentive force. J Prosthodont Res. 2015;59(2):136-143.
3. El Kerdani T, Roushdy S. The Use of CAD/CAM Technology for Fabricating Cast Gold Survey Crowns under Existing Partial Removable Dental Prosthesis. A Clinical Report. J Prosthodont. 2017;26(4):321-326.
4. Paek J, Noh K, Pae A, Lee H, Kim HS. Fabrication of a CAD/CAM monolithic zirconia crown to fit an existing partial removable dental prosthesis. J Adv Prosthodont. 2016;8(4):329-332.
5. Lee JH. Fabricating a crown under an existing removable partial denture with impression scanning and CAD-CAM technology. J Prosthet Dent. 2020;124(2):148-152.
6. Gouveia DNM, Razzoog ME, Alfaro MF. A fully digital approach to fabricating a CAD-CAM ceramic crown to fit an existing removable partial denture. J Prosthet Dent. 2019;121(4):571-575.
7. Tran CD, Sherraden DR, Curtis TA. A review of techniques of crown fabrication for existing removable partial dentures. The Journal of Prosthetic Dentistry. 1986;55(6):671-673.
8. Petre AE, Macris A, Spinu TC, Smarandache AM. Fully digital workflow for retrofitting a new crown to an existing removable partial denture. J Prosthet Dent. Published online March 29, 2023:S0022-3913(23)00133-6.
9. Tasaka A, Shimizu T, Hirabayashi T, Yamashita S. Fabrication of Zirconia Abutment Crown and Clasp Under Existing Removable Partial Denture Using CAD/CAM Technology. Clin Cosmet Investig Dent. 2021;13:421-427.
10. Smith CS, Grandin H, Low K. A predictable all-digital workflow to retrofit a crown to an existing removable prosthesis. J Prosthet Dent. 2019;121(6):876-878.
11. Statement on ASA Physical Status Classification System. Accessed March 6, 2024. https://www.asahq.org/standards and-practice-parameters/statement-on-asa-physical-status-classification-system
12. Kim JJ. Revisiting the Removable Partial Denture. Dental Clinics. 2019;63(2):263-278.
13. Deng F. American Dental Association Universal Numbering System | Radiology Reference Article | Radiopaedia.org. Radiopaedia.
14. Caton JG, Armitage G, Berglundh T, et al. A new classification scheme for periodontal and peri-implant diseases and conditions – Introduction and key changes from the 1999 classification. Journal of Periodontology. 2018;89(S1):S1-S8.
15. Chochlidakis KM, Papaspyridakos P, Geminiani A, Chen CJ, Feng IJ, Ercoli C. Digital versus conventional impressions for fixed prosthodontics: A systematic review and meta-analysis. The Journal of Prosthetic Dentistry. 2016;116(2):184-190.e12.
This article licensed under the Creative Commons Attribution 4.0 International License CC-BY 4.0., which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are properly credited.