NL Journal of Dentistry and Oral Sciences
(ISSN: 3049-1053)
The Role of Dentistry in Obstructive Sleep Apnea (OSA) – Clinical Review
Author(s) : Tahira Hussain, Muhammad Anas. DOI : 10.71168/NDO.02.03.119
Abstract
Obstructive sleep apnea (OSA) is a prevalent sleep disorder characterized by recurrent upper airway collapse during sleep, leading to hypoxia, sleep fragmentation, and systemic sequelae. Dentists play a pivotal role in OSA management through screening, oral appliance therapy (OAT), and interdisciplinary collaboration. This review synthesizes current evidence on dental interventions for OSA, emphasizing diagnostic limitations, therapeutic efficacy, and evolving practice guidelines. While OAT is effective for mild-to-moderate OSA, diagnosis remains the purview of sleep physicians. Controversies regarding dental scope expansion and the need for standardized training are discussed. Keywords: Obstructive sleep apnea, oral appliance therapy, dental sleep medicine, interdisciplinary care, mandibular advancement devices
Introduction
Obstructive Sleep Apnea (OSA) is a sleep breathing disorder characterized by frequent upper airway obstructions, which result in partial or complete obstruction of airflow, lowering oxygen levels, and disturbances in sleep patterns [1]. This condition causes fragmented and poor-quality sleep, resulting in excessive daytime sleepiness, fatigue, and loss of productivity. Other symptoms include loud snoring, sleep breathing pauses, and morning headaches [2]. The impact of OSA transcends sleep disturbances and affects cardiovascular health, mental health, daily functioning, and driving capacity, ultimately impacting overall quality of life [3]. OSA is a common sleep disorder that has a considerable health burden, including greater morbidity, mortality, and diminished quality of life [4]. [Figure 1]
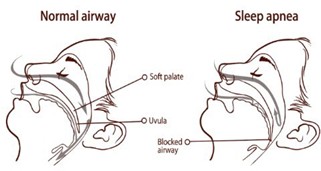 Figure 1: Reprinted from Diva Dentistry. Obstructive sleep apnea (OSA) and oral appliances [17]
Figure 1: Reprinted from Diva Dentistry. Obstructive sleep apnea (OSA) and oral appliances [17]
Continuous positive airway pressure (CPAP) is the gold-standard therapy for sleep apnea owing to its high effectiveness in decreasing apneic episodes. Nonetheless, its long-term success relies on the patient’s compliance, which is restricted by distress and compliance problems. For individuals who find it difficult to use CPAP, oral appliance therapy (OAT) presents a useful and more acceptable option [5]. The design and fitting of an oral appliance therapy (OAT) device are specialized tasks that can only be done by a trained dentist, as advocated by professional groups in sleep medicine and dental sleep practice [6].
Dentists have played a crucial role in the collaborative assessment and treatment of patients with Obstructive Sleep Apnea (OSA) with oral appliances, with roots tracing back to the 1980s and formal practice parameters in 1995 [7]. As dentistry became increasingly engaged in OSA treatment, controversy arose over the scope of practice of the profession. The key issues are whether or not dentists can treat snoring patients autonomously and the need for medical supervision of OAT prescriptions [8]. Although some tensions between medicine and dentistry remain, important strides have been made in delineating the dentist’s role in assessing and treating patients with Obstructive Sleep Apnea (OSA). Guidelines from the American Academy of Sleep Medicine (AASM) and the American Academy of Dental Sleep Medicine (AADSM), joined together in a joint statement, and an AADSM treatment protocol have served to establish firm parameters for interdisciplinary treatment [6]. Dentists play a vital role in identifying patients with Obstructive Sleep Apnea (OSA). During routine dental exams, they can recognize anatomical risk factors, such as a narrow upper airway, and utilize simple screening tools, including questionnaires, to pinpoint potential OSA patients [9]. While dentists play a crucial role in identifying potential signs of obstructive sleep apnea (OSA), the formal diagnosis should be made by physicians, particularly sleep specialists, who have the expertise to assess its interaction with other medical conditions [10].
Dentists are integral in assessing patients with OSA for the appropriateness of oral appliance therapy (OAT), selecting the most suitable device, making necessary adjustments, and monitoring for potential side effects [8]. Effective management requires close collaboration between dentists and sleep medicine physicians, ensuring patients receive the most comprehensive and effective treatment for their OSA. Within the profession of dentistry, there has been increasing momentum to increase the role of the dentist in the diagnosis and treatment of OSA beyond the standard guidelines and protocols [11]. This is supported by anecdotal case reports, marketing materials [12], and efforts to change scope of practice laws. In Texas, after extensive deliberation, the State Board of Dental Examiners decreed that dentists cannot diagnose OSA on their own and can only prescribe oral appliance therapy (OAT) in conjunction with a physician.16 Yet, even after protests by the Texas Medical Association [13], there is no clear mention of other sleep disorders, how to interpret sleep studies, or how sleep diagnostic tools are to be dispensed. At the same time, the Colorado Dentistry Board is involved in policy formulation about how dentists can participate in OSA diagnosis and treatment [14].
Both sleep physicians and qualified dentists play crucial roles in managing OSA with oral appliance therapy (OAT) [6,8]. Enhancing pediatric dental education and advancing digital dental technologies may further support OSA management [15,16]. The sleep physician is responsible for confirming the diagnosis and determining if OAT is a suitable option, while the dentist assesses its appropriateness and initiates treatment. Ongoing follow- up should involve both professionals, leveraging their respective expertise. Establishing a strong collaborative relationship between dentists and sleep physicians is essential to ensure patients receive the most effective and comprehensive care for their OSA.
Dental Screening and Diagnosis in OSA
Dentists serve as valuable frontline screeners for OSA by utilizing validated instruments like the STOP-Bang questionnaire and Epworth Sleepiness Scale, combined with clinical assessment of anatomical risk factors, including Mallampati score and tonsillar hypertrophy [18]. However, it must be emphasized that formal diagnosis requires confirmation through polysomnography or home sleep apnea testing (HSAT) under physician supervision [19].
Significant oral health correlations with OSA have been well-documented:
- Bruxism: Present in 25-50% of OSA patients, often serving as a clinical marker for sleep-disordered breathing [20].
- Periodontal disease: The chronic inflammatory state induced by intermittent hypoxia appears to exacerbate periodontal pathology [21].
- Xerostomia: Mouth breathing associated with OSA leads to decreased salivary flow, increasing susceptibility to dental caries and other oral complications [22].
These oral manifestations provide important clinical indicators that can aid in the early identification of at-risk patients during routine dental examinations. The dental professional’s role in recognizing these signs facilitates timely referral for comprehensive sleep evaluation while maintaining appropriate professional boundaries in diagnosis.
Oral Appliance Therapy (OAT) in OSA Management
Oral appliance therapy has emerged as an effective treatment option for obstructive sleep apnea, particularly through the use of mandibular advancement devices (MADs), which are custom-fitted to protrude the mandible and stabilize the upper airway, demonstrating an AHI reduction of 50–60% [9,12]. While tongue-retaining devices represent an alternative approach, their clinical use remains limited due to patient-reported discomfort and dry mouth [12]. [Figure 2].
 Figure 2: Reprinted from Diva Dentistry. Obstructive sleep apnea (OSA) and oral appliances [17]
Figure 2: Reprinted from Diva Dentistry. Obstructive sleep apnea (OSA) and oral appliances [17]
OAT is primarily indicated for patients with mild-to-moderate OSA or those with severe OSA who are intolerant of CPAP therapy [9,12]. Treatment success is typically defined by either a reduction in AHI to fewer than 10 events per hour or a 50% improvement from baseline [9]. However, clinicians must remain vigilant about potential adverse effects, including occlusal changes (occurring in 15–20% of patients) and temporomandibular joint (TMJ) pain, which necessitate careful patient selection and long-term monitoring [10]. Given its favorable efficacy and patient compliance profile, OAT represents a valuable therapeutic alternative within a comprehensive, multidisciplinary approach to OSA management.
Interdisciplinary Collaboration in OSA Management
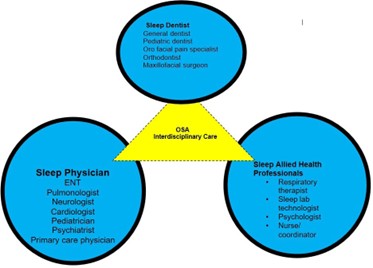
The management of obstructive sleep apnea requires close collaboration between dental professionals and sleep physicians, as emphasized by guidelines from both the American Academy of Sleep Medicine (AASM) and the American Academy of Dental Sleep Medicine (AADSM). A fundamental principle of this partnership is that diagnosis must remain physician-led, with dentists playing a crucial but limited role in screening while deferring formal diagnosis and sleep study interpretation to qualified sleep specialists [6]. The optimal approach follows a shared care model, where sleep physicians determine the appropriateness of oral appliance therapy (OAT) and prescribe treatment, while dentists take responsibility for device selection, customization, fitting, and long-term management of therapy-related side effects [2,10]. However, this collaborative framework has faced challenges in some jurisdictions, where dental boards (notably in Texas and Colorado) have considered expanding dentists’ roles to include home sleep apnea test (HSAT) administration. These proposals have met with opposition from medical societies, who argue that such expansions exceed the scope of dental training and could compromise diagnostic accuracy [19,20]. These ongoing debates highlight the need for clear professional boundaries while reinforcing the importance of interdisciplinary cooperation to ensure optimal patient outcomes in OSA management. The current evidence strongly supports maintaining this physician-dentist partnership, with each profession contributing its unique expertise within well-defined roles.
Future Directions
The evolving landscape of dental sleep medicine presents several promising avenues for improving obstructive sleep apnea (OSA) management [24]. Enhanced dental education [15] is critical, as current training in sleep disorders remains limited in many dental programs. Integrating comprehensive sleep medicine modules into dental curricula-covering screening protocols, oral appliance therapy (OAT) indications, and interdisciplinary collaboration-would better equip dentists to recognize and manage OSA effectively. Additionally, pediatric OSA interventions warrant greater attention, given the growing evidence supporting early intervention. Orthodontic approaches such as rapid maxillary expansion (RME) and myofunctional therapy have shown potential in improving airway dimensions and reducing OSA severity in children, which may prevent long-term neurocognitive and cardiovascular complications [23]. Technological advancements are also reshaping treatment paradigms, with 3D printing and digital imaging [16] enabling more precise fabrication of custom oral appliances, while telemedicine platforms [24] facilitate remote monitoring of patient compliance and therapeutic efficacy. Together, these developments highlight the need for ongoing innovation, standardized training, and collaborative research to optimize OSA care across all age groups.
Conclusion
Dentists play a crucial role in managing OSA through screening, oral appliance therapy, and interdisciplinary collaboration. While CPAP remains the gold standard, OAT provides an effective alternative for mild-to-moderate cases, especially for CPAP-intolerant patients. Successful treatment requires close cooperation between dentists and sleep physicians to ensure accurate diagnosis and optimal care. Future advancements in education, pediatric interventions, and digital dentistry promise to further enhance OSA management. By adhering to evidence-based guidelines and maintaining strong professional partnerships, dental professionals can significantly improve outcomes for OSA patients.
References
1. Slowik JM, Sankari A, Collen JF. Obstructive Sleep Apnea. 2022. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. 2023.
2. Carneiro-Barrera A, Díaz-Román A, Guillén-Riquelme A, Buela-Casal G. Weight loss and lifestyle interventions for obstructive sleep apnoea in adults: Systematic review and meta-analysis. Obes Rev. 2019 May;20(5):750-762.
3. Yeghiazarians Y, Jneid H, Tietjens JR, Redline S, Brown DL, El-Sherif N, Mehra R, Bozkurt B, Ndumele CE, Somers VK. Obstructive Sleep Apnea and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2021 Jul 20;144(3):e56-e67
4. Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MS, Morrell MJ, Nunez CM, Patel SR, Penzel T, Pépin JL, Peppard PE. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. The Lancet respiratory medicine. 2019 Aug 1;7(8):687-98.
5. Zhu Y, Long H, Jian F, et al. The effectiveness of oral appliances for obstructive sleep apnea syndrome: a meta-analysis. J Dent. 2015;43:1394–1402.
6. American Academy of Sleep Medicine; American Academy of Dental Sleep Medicine. Policy Statement on the Diagnosis and Treatment of OSA. American Academy of Dental Sleep Medicine website. [Accessed March 23, 2025]. http://aadsm.org/osapolicystatement.aspx. Published December 7, 2012.
7. Quan SF, Schmidt-Nowara W. The role of dentists in the diagnosis and treatment of obstructive sleep apnea: consensus and controversy. Journal of Clinical Sleep Medicine. 2017 Oct 15;13(10):1117-9.
8. Ramar K, Dort LC, Katz SG, et al. Clinical practice guideline for the treatment of obstructive sleep apnea and snoring with oral appliance therapy: an update for 2015. J Clin Sleep Med. 2015;11(7):773–827.
9. Lavanya R, Gandhi Babu DB, Chavva S, Boringi M, Waghray S, Yeladandi M. The role of oral physicians in predicting the risk of obstructive sleep apnea: a case-control study. Imaging Sci Dent. 2016;46(3):167–171.
10. Rosen IM, Kirsch DB, Chervin RD, et al. Clinical use of a home sleep apnea test: an American Academy of Sleep Medicine position statement. J Clin Sleep Med. 2017;13(10):1205–1207.
11. Dioguardi AT. Incorporating Home Sleep Testing into Oral Appliance Therapy. Sleep Review website. [Accessed : March 23, 2025]. http://www.sleepreviewmag.com/2016/07/home-sleep-testing-oral-appliance-therapy. Published July 4, 2016.
12. DORA Colorado. Colorado Dental Board Stakeholder Meeting (Sleep apnea #1) YouTube website. [Accessed: March 23, 2025]. https://www.youtube.com/watch?v=PZrbaHUQkfw&feature=youtu.be. Published April 7, 2017.
13. Texas State Board of Dental Examiners. Rules and Regulations, 108.12, Dental Treatment of Obstructive Sleep Apnea. Texas Secretary of State website. [Accessed March 23, 2025].http://texreg.sos.state.tx.us/public/readtac$ext. Published 2017.
14. Texas Medical Association. TMA Opposes Dental Board’s Sleep Apnea Treatment Rules. Texas Medical Association website. [Accessed March 23, 2025]. https://www.texmed.org/Template.aspx?id=36189. Published May 2, 2016.
15. Anas M, Ullah I, Sultan MU. Enhancing paediatric dental education: a response to curriculum shifts. European Archives of Paediatric Dentistry. 2024 Nov 22:1-2.
16. Anas M, Ullah I, Usman Sultan M. Embracing the future: integrating digital dentistry into undergraduate dental curriculum. Journal of the California Dental Association. 2024 Dec 31;52(1):2422144.
17. Diva Dentistry. Obstructive sleep apnea (OSA) and oral appliances [Internet]: Diva Dentistry; [cited 2025 Mar 25]. Available from: https://www.divadentistry.com/obstructive-sleep-apnea-osa-and-oral-appliances/
18. Kale SS, Kakodkar P, Shetiya SH. Assessment of oral findings of dental patients who screen high and no risk for obstructive sleep apnea (OSA) reporting to a dental college - A cross sectional study. Sleep Science. 2018;11(2):112-117. doi: 10.5935/1984-0063.20180021.
19. Hussein O, Alkhader A, Gohar A, Bhat A. Home Sleep Apnea Testing for Obstructive Sleep Apnea. Missouri Med. 2024;121(1):60-65.
20. Martynowicz H, Gac P, Brzecka A, Poreba R, Wojakowska A, Mazur G, et al. The Relationship between Sleep Bruxism and Obstructive Sleep Apnea Based on Polysomnographic Findings. J Clin Med. 2019;8(10):1653. doi: 10.3390/jcm8101653.
21. Kim SR, Son M, Kim YR. Risk of chronic periodontitis in patients with obstructive sleep apnea in Korea: a nationwide retrospective cohort study. Epidemiol Health. 2023;45:e2023032. doi: 10.4178/epih.e2023032.
22. Maniaci A, Lavalle S, Anzalone R, Lo Giudice A, Cocuzza S, Parisi FM, et al. Oral Health Implications of Obstructive Sleep Apnea: A Literature Review. Biomedicines. 2024;12(7):1382. doi: 10.3390/biomedicines12071382.
23. Correa LP, Acosta-Torres LS. The Evolving Field of Dental Sleep Medicine. Dent Clin North Am. 2024;68(3):429-441. doi:10.1016/j.cden.2024.02.001.
24. Vudathaneni VK, Lanke RB, Mudaliyar MC, Movva KV, Mounika Kalluri L, Boyapati R. The Impact of Telemedicine and Remote Patient Monitoring on Healthcare Delivery: A Comprehensive Evaluation. Cureus. 2024;16(3):e55534. doi:10.7759/cureus.55534.
This article licensed under the Creative Commons Attribution 4.0 International License CC-BY 4.0., which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are properly credited.