NL Journal of Dentistry and Oral Sciences
(ISSN: 3049-1053)
Oral Care Challenges in Hypophosphatemic Vitamin D-Resistant Rickets (VDRR): A Case Report
Author(s) : Boudi Rachid, Ramdi Hind, Majid Sakout, Elalloussi Mustapha. DOI : 10.71168/NDO.02.02.111
Abstract
Hypophosphatemia due to vitamin D resistant rickets is a genetic condition that involves problems with phosphate use, which causes difficulties in properly mineralizing bones and teeth. The typical clinical characteristics include bowing of the lower extremities, short stature, scoliosis, and beading at the rib-sternal junction. Dental findings of this condition include enlarged pulp chambers, pulp horns that spread outside the dentino- enamel junction, enamel and dentine defects, poorly defined lamina-dura, short roots and a hypoplastic alveolar ridge. The therapeutic approach consists of the prevention of dental infectious complications by prophylactic care. This can be achieved on temporary teeth by prophylactic pulp treatment, pulpotomy, pulpectomy, preformed stainless steel pedodontics cap and/or by composite resin and glass ionomer cement. This article presents the dental management of a child 4 years old with Hypophosphatemia and vitamin D resistance. Keywords: Rickets, dental pulp, hypophosphatemia, child, vitamin D.
Introduction
Hypophosphatemia due to Vitamin D-resistant rickets is a genetic disease that involves problems with phosphate, leading to difficulty in properly mineralizing bones and teeth [1,2,3].
The effects of this disease called vitamin D-resistant hypophosphatemia rickets on bone and dental health are serious and complex. Among the most important problems associated with X-linked hypophosphatemia rickets (XLH) is the high prevalence of bone deformities and dental problems [4,5].
Clinical problems of vitamin D-resistant hypophosphatemic rickets are intricately associated with genetic abnormalities in the PHEX gene, which disrupt phosphate metabolism. This results in increased concentrations of fibroblast growth factor 23 (FGF23), which inhibits renal phosphate reabsorption, causing decreased phosphate levels in the body and bone hypomineralization [6,7,8].
The compromised odontogenesis associated with this condition increases the risk of individual caries through increased Cario-susceptibility and leads to delayed dental eruption and oral dysmorphosis [3,5]. the therapeutic approach for these patients requires the cooperation of several disciplines for optimal clinical results, including pediatric dentistry and close medical monitoring.
This medical approach takes into consideration both immediate dental problems and possible long-term complications of rickets on the oral and overall health of the child, within the framework of the different stages of oral prevention: primary, secondary and tertiary.
This paper provides the clinical and radiographic dental aspects of a case from our pediatric dentistry department.
Case Report
A 4-year-old boy was referred to our pediatric dentistry department with a complaint of fistula in the mandibular area.
Upon anamnesis, the patient was diagnosed with hypophosphatemia and vitamin D-resistant rickets.
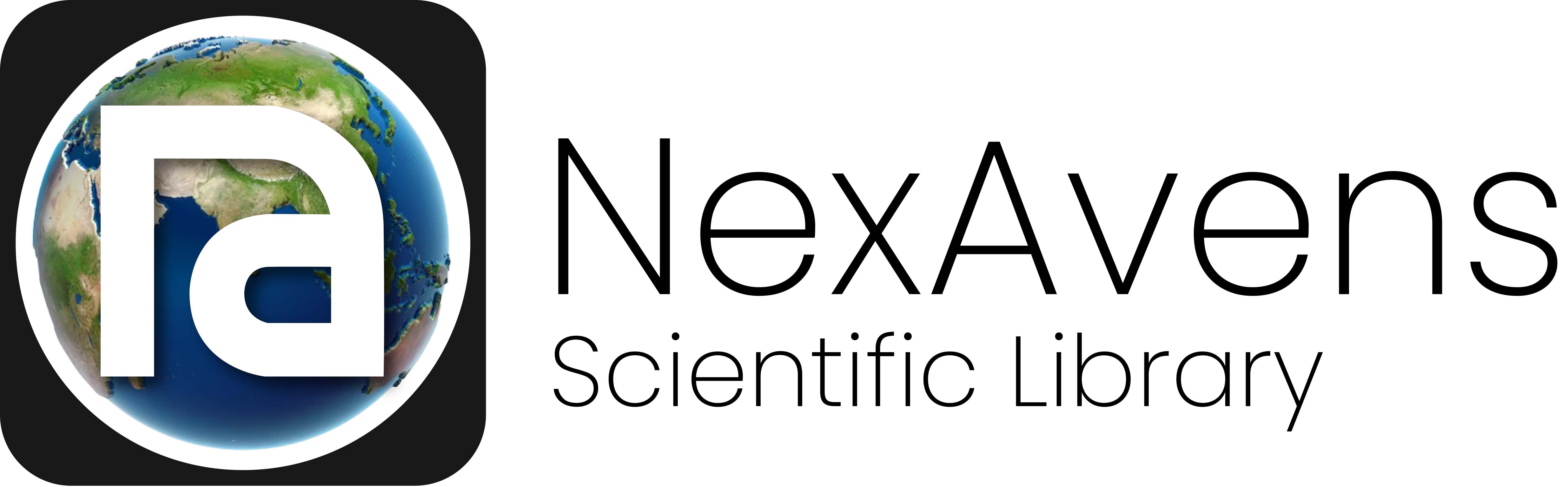
The patient had short height, minor frontal and occipital bossing, bending of the lower limbs, broadening of the wrists and ankles, and a rachitic deformity (Figures 1, 2, and 3).
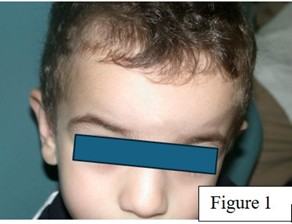
Figure 1: Frontal bossing

Figure 2,3: Flexion of the lower limbs
The clinical dental examination indicated the presence of a fistula in the periodontal area of the mandibular right central incisor (figure 4), with no evidence of caries or trauma (figures 5, 6).
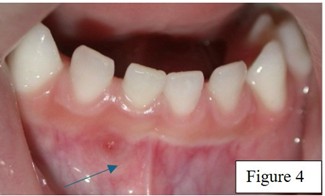
Figure 4: Clinical examinations revealed a fistula at the periapical region of primary mandibular right central incisor

Figure 5,6: The patient presented with complete primary dentition and none of the teeth examined showed evidence of caries or trauma
Minor mobility of the primary incisor was seen; however, a maxillary occlusal radiograph showed no evidence of periodontal pathosis.
After informed consent was obtained, a pulpectomy procedure was commenced. The access cavity was created using rubber dam isolation. Necrotic pulp tissue was excised, and the working length was determined.
The canal was cleaned and shaped using pediatric nickel-titanium rotary instruments. A calcium hydroxide dressing was applied for 10 days. At the second appointment, the fistula disappeared (figure 7,8) and the canal was obturated using zinc-oxide eugenol (figure 9).
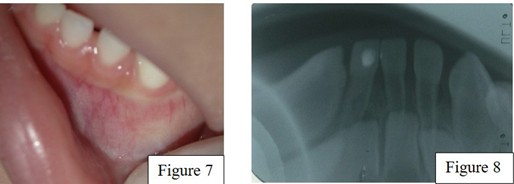
Figure 7,8: Isparition of the fistula after implementation as intracanal medication with calcium hydroxide for 10 days
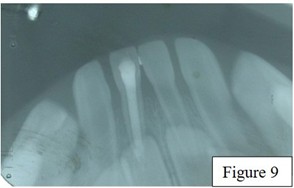
Figure 9: Pulpectomy of the mandibular right central incisor
X-ray examination revealed enlarged pulp chambers, pulp horns extending beyond the dentino-enamel junction, abnormalities in enamel and dentine, poorly defined lamina-dura, short roots and hypoplastic alveolar ridge (figure 10).
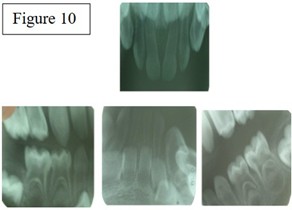
Figure 10: Periapical radiography showed pulp chambers enlarged with pulp horns extending to the dentino-enamel Junction
Finally, oral hygiene measures were ultimately administered to the patient and his parents. Topical fluoride varnish was administered to all the teeth to avoid probable pulp pathologies and the patient had periodic follow-ups.
Discussion
Hypophosphatemic rickets is a category of genetic illnesses characterized by impaired renal phosphate control, exhibiting closely related symptoms and three recognized modes of inheritance: autosomal dominant (ADHR), autosomal recessive (ARHR) and X-linked dominant (XLH), with the latter being the most common form [2].
Vitamin D resistant rickets (VDRR) are also called as X-linked hypophosphatemia with a prevalence of 1:20000 people [3].
The standard clinical features of VDRR include short stature, lower extremity bending, scoliosis, and beading at the rib-sternal junction, referred to as the rachitic rosary [9].
Bone metabolic abnormalities result in distinct clinical and systemic features, which may differ across individuals owing to several circumstances, including the age of illness onset, familial history, severity of hypophosphatemia, and timing of medication commencement.
The clinical manifestations of HR at the craniofacial level are individual and, in many instances, may remain undetected due to the advancement of its systemic manifestations [10].
The relationship between genes and vitamin D use plays a major role in the severity of vitamin D resistant rickets, particularly in terms of dental health. Genetic differences in the vitamin D receptor (VDR) and enzymes that help make and break down vitamin D, such as CYP27B1 and CYP24A1, can cause different reactions to vitamin D supplements and affect how bones absorb minerals (Amlani et al.) [11].
Mutations in the PHEX cause this disorder, resulting in higher levels of fibroblast growth factor 23 (FGF23). This factor is important for phosphate use and leads to various health issues, including dental problems (Ariceta Iraola et al.) [12].
Studies have shown that the use of active vitamin D metabolites might help with some bone deformities, but it is still unclear whether this treatment directly helps dental health.
Clinical signs of dental issues in patients with Vitamin D-resistant rickets are complicated. Studies have shown that these patients often have major dental problems, such as enamel hypoplasia, unusual dentin structure that features thin globular dentin, and large pulp horns and chambers, which make them more prone to pulpitis and periapical abscesses.
Dental findings in this syndrome include larger pulp chambers, pulp horns extending beyond the dentino-enamel junction, enamel and dentin abnormalities, poorly defined lamina dura, shortened roots, and a hypoplastic alveolar ridge [3].
Malocclusion linked to hypophosphatemic rickets is present; however, it has not been documented. An open bite is the most prevalent anomaly seen, attributable to a deficit in maxillary development relative to mandibular growth [2].
Hypoplasia resulting from vitamin D insufficiency has a distinctive manifestation known as chronological hypoplasia. Hypoplastic enamel manifests as bands on the crowns of the teeth, reflecting the period of enamel formation. Upon rectification of the deficit, enamel synthesis resumes its normalcy [11].
The therapeutic approach consists of the prevention of dental infectious complications by prophylactic care. This can be achieved on temporary teeth by prophylactic pulp treatment, pulpotomy, pulpectomy, preformed stainless steel pedodontic cap, and/or by composite resin and glass ionomer cement [10].
Patients with VDRR should get qualified dental treatment, including regular exams and preventative oral hygiene practices. Consequently, dentists are encouraged to provide information on the dental traits that may first identify such patients and to obtain recommendations to dental specialists promptly to avert dental infections [10].
Pit and fissure sealants are effective upon tooth eruption since they inhibit bacterial entry into enamel microfractures and the onset of caries in deep pits and fissures [2].
Conclusion
Treating primary teeth in children with vitamin D-resistant rickets requires a comprehensive approach that accounts for the disease’s impact on the body and dentition.
Early and preventive dental care is crucial because these dental disorders may exacerbate overall health difficulties. Additionally, because vitamin D deficiency results in enamel hypoplasia, making dental care more difficult, its consequences extend beyond general health.
Therefore, a comprehensive treatment strategy that incorporates preventative care, routine dental examinations, and family education initiatives is essential to improving the oral health and quality of life of children with Vitamin D resistant rickets.
References
1. Melissa Almeida Souza, Luiz Alberto Valente Soares Junior, Marcela Alves dos Santos, Maria Helena Vaisbich. “Dental abnormalities and oral health in patients with hypophosphatemic rickets”. CLINICS 2010;65(10):1023-1026
2. Souza, M. A., Soares Junior, L. A. V., Santos, M. A. dos, & Vaisbich, M. H. (2010). Dental abnormalities and oral health in patients with Hypophosphatemic rickets . Clinics, 65(10), 1023-1026
3. Akif Demirel, Ayşe Tuba Altuğ, Esra Erdemli, Firdevs Tulga Oz. “Dental Management of Hypophosphatemic Vitamin D Resistant Rickets”. Journal of Pediatric Research 2018;5(4):221-4
4. Godfrey EK, Mussa F, Kazahura P, Shoo A, Naburi H, Manji KP. Vitamin D-Resistant Rickets Diagnostics and Treatment Challenges at Muhimbili National Hospital, Tanzania. Case Rep Endocrinol. 2020 Jan 28;2020:1547170.
5. Lee BN, Jung HY, Chang HS, Hwang YC, Oh WM. Dental management of patients with X-linked hypophosphatemia. Restor Dent Endod. 2017 May;42(2):146-151.
6. Park E, Kang HG. X-linked hypophosphatemic rickets: From diagnosis to management. Clin Exp Pediatr. 2024 Jan;67(1):17-25.
7. Wolf M. Update on fibroblast growth factor 23 in chronic kidney disease. Kidney Int. 2012 Oct;82(7):737-47.
8. Lecoq AL, Brandi ML, Linglart A, Kamenický P. Management of X-linked hypophosphatemia in adults. Metabolism. 2020 Feb;103S:154049
9. Rakocz M, Keating J 3rd, Johnson R. Management of the primary dentition in vitamin D-resistant rickets. Oral Surg Oral Med Oral Pathol. 1982 Aug;54(2):166-71
10. Janet Ofelia Guevara-Canales,Nathali Cardenas-Zuñiga,Miguel Chavez-Pastor,Milana Trubnykova,Rafael Morales-Vadillo Prevalence of oral manifestations of hypophosphatemic rickets in patients treated in a Peruvian Pediatric Hospital. October 2020 journal of oral research 9(5):383-391
11. Price DK, Franks ME, et al. Genetic variations in the vitamin D receptor, androgen receptor and enzymes that regulate androgen metabolism. J Urol. 2004 Feb;171(2 Pt 2):S45-9; discussion S49.
12. Carpenter TO,Feingold KR, Anawalt B, Blackman MR, Boyce A, Chrousos G, Corpas E, de Herder WW, Dhatariya K, Dungan K, Hofland J, Kalra S, Kaltsas G, Kapoor N, Koch C, Kopp P, Korbonits M, Kovacs CS, Kuohung W, Laferrère B, Levy M, McGee EA, McLachlan R, New M, Purnell J, Sahay R, Shah AS, Singer F, Sperling MA, Stratakis CA, Trence DL, Wilson DP. Primary Disorders of Phosphate Metabolism. Endotext [Internet]. South Dartmouth (MA)
This article licensed under the Creative Commons Attribution 4.0 International License CC-BY 4.0., which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are properly credited.