NL Journal of Medical and Pharmaceutical Sciences
(ISSN: 3108-0502)
Call for Enhancing Pregnant Women’s Knowledge Regarding Teratogenic Medications and Most Common Drugs That Cause Congenital Anomalies
Author(s) : Heba Ahmed Mohamed, Hanan Elzeblawy Hassan*, Hagar Kamal Masoud. DOI : 10.71168/NMP.01.03.114
Abstract
Background: Self-medication presents serious health risks for pregnant women and their fetuses, warranting global concern. Historical incidents, like the thalidomide crisis, emphasize the importance of evaluating the risks tied to medication use during pregnancy. Aim: The current study was conducted to evaluate the effect of an educational program on enhancing pregnant women’s knowledge regarding teratogenic medications and the most common drugs that cause congenital anomalies. Subjects and Methods: Design: A quasi-experimental design was used. Sample and Settings: A convenient sample of 358 pregnant women was used at outpatient clinics at Beba Hospital, affiliated with the Ministry of Health, Beni-Suef Governorate. Tools: Tool 1: A structured interview questionnaire. Tool 2: Women’s knowledge regarding congenital anomalies and the drug that causes women to fill out a questionnaire sheet. Tool 3: A questionnaire sheet assessing women’s knowledge about the most common drugs that cause congenital anomalies. Results: reveal that 46.6% of women had previous births through cesarean section and 27.4% had normal vaginal births; 70.9%, 63.1%, and 67.3% of women had correct knowledge of medication, prescription, and current use. Additionally, 46.9% and 47.8% of women had correct knowledge about congenital malformations and medications that do not cause anomalies. Moreover, the study revealed that 86.3% of women had inadequate knowledge about congenital anomalies and their causes, which regressed to 17.0% posttest and 21.8% posttest, respectively. Conclusion: The study also showed improvements in understanding common drugs that cause congenital anomalies, such as Imodium, Anabril, and clonazepam, which improved posttest. Additionally, the study found that pregnant women with correct knowledge of medication and congenital anomalies during pregnancy showed significant improvement posttest. The posttest significantly improved compared to the pretest. Recommendation: Collaborate with public health organizations to implement national awareness programs focusing on educating pregnant women about teratogenic medications and offering resources for safer pregnancy practices. Keywords: Enhancing, Knowledge, Teratogenic Medications, Drugs, Congenital Anomalies.
Introduction
Teratogenic drugs are medications or chemical substances that can interfere with fetal development during pregnancy, leading to congenital abnormalities or other adverse outcomes. These drugs pose the greatest risk during the embryonic period, particularly between weeks 3 and 8 post-conception, which is especially sensitive to external influences, and exposure to teratogens during this time can lead to disorders in organ differentiation and, consequently, malformations. Understanding the impact of these factors on the organogenesis process is essential, as it provides a basis for addressing and preventing potential complications in fetal development [1].
Several antiepileptic drugs (AEDs) are known to have teratogenic effects. Valproic acid, for example, is associated with neural tube defects like spina bifida, as well as craniofacial abnormalities and heart defects. Similarly, phenytoin has been linked to fetal hydantoin syndrome, characterized by growth deficiencies, facial abnormalities, and developmental delays. Carbamazepine, another common antiepileptic drug (AED), carries a risk of neural tube defects and minor facial deformities. Pregnant women taking antiepileptic drugs require careful management to minimize risks [1].
Retinoid medications, commonly used for severe acne or psoriasis, are among the most teratogenic drugs. Isotretinoin can cause severe craniofacial, cardiac, and central nervous system abnormalities. Even small doses can result in fetal malformations, making it critical for individuals on isotretinoin to use effective contraception. Acitretin, used for psoriasis, has long-lasting teratogenic effects that may persist even after discontinuation, necessitating extended contraceptive measures [2].
Warfarin, a commonly used anticoagulant, can cause fetal warfarin syndrome, characterized by nasal hypoplasia, limb defects, and central nervous system abnormalities. Similarly, drugs like thalidomide, famous for its history of causing limb deformities, and angiotensin-converting enzyme (ACE) inhibitors, which can lead to kidney and growth abnormalities [2].
Preconception counseling can significantly reduce maternal and infant morbidity and mortality by optimizing health before pregnancy [3-5]. This involves a thorough review of current medications to review medications for safety, efficacy, and possible dosing adjustments; taking a careful family history; providing genetic counseling; and offering patients genetic screening [6-8]. Assess immunization status and offer patients appropriate vaccinations. In addition, providing appropriate patient education on diet and nutrition and supplements may reduce risks to the fetus, especially in early pregnancy before the first prenatal visit, thereby establishing a foundation for a healthier pregnancy [9-12].
Preconception care is vital by focusing on the preconception period that nurses provide to women planning a pregnancy. During these sessions, interventions such as optimizing nutrition, managing chronic medical conditions, ensuring vaccinations are current, identifying and addressing genetic risks, and promoting healthy lifestyle choices are used. Addressing these factors and optimizing health before pregnancy can significantly contribute to the well-being of both the mother and the developing fetus. It can reduce the risk of pregnancy complications, birth defects, and other adverse outcomes [13-17].
During pregnancy, nurses work closely with the healthcare team to ensure patients receive tailored care plans. For example, pregnant women with epilepsy may require a balance between seizure control with anti-epilepsy medications and the adverse drug effects on mothers and fetuses. Taking ASMs has an increased risk of some maternal and delivery complications, including preeclampsia, vaginal bleeding, labor induction, and the need for cesarean section. Nurses advise pregnant women to use folic acid supplements before and during pregnancy to reduce antiepileptic drug side effects [18].
Lifestyle modifications are essential for reducing teratogenic risks. Pregnant women should avoid alcohol completely, as even small amounts can lead to fetal alcohol spectrum disorders. Smoking cessation is also crucial, as tobacco increases the risk of low birth weight, preterm birth, and other complications. Recreational drugs like cocaine, marijuana, and opioids should be strictly avoided, as they have been linked to severe developmental and neurological problems in the fetus [19-22].
Drugs like cocaine, methamphetamine, and opioids are associated with severe neonatal complications, including withdrawal syndromes, low birth weight, and developmental delays. Pregnant women should also maintain balanced diet, as deficiencies in nutrients like iodine, iron, and vitamin D can negatively affect fetal development [23].
Nurses advocate for safe environments at home and work. Nurses educate pregnant women about avoiding harmful substances like pesticides, solvents, and cleaning chemicals. Nurses guide patients on workplace safety, including the use of personal protective equipment and discussing job modifications if necessary [24].
Aim of the Study
The current study was conducted to evaluate the effect of an educational program on enhancing pregnant women’s knowledge regarding teratogenic medications and the most common drugs that cause congenital anomalies.
Research Hypothesis
Pregnant women’s knowledge regarding teratogenic medications and the most common drugs that cause congenital anomalies will be improved after implementation of the educational program.
Subject and Method
Research Design: Quasi-experimental research design (pre/post-test) was utilized.
Subjects and Settings: A convenient sample of 358 pregnant women was used at outpatient clinics at Beba Hospital, affiliated with the Ministry of Health, Beni-Suef Governorate.
Tools of Data Collection
Tool 1: A structured interview questionnaire: A self-administered questionnaire was designed for data collection. An Arabic-structured interview was developed after a thorough literature review, incorporating open- and closed- end questions regarding reproductive history to meet the study’s objectives and data requirements.
Tool 2: Women’s knowledge regarding congenital anomalies and the drug that causes women questionnaire sheet: Total global score from 21 questions, each worth 1 point, was calculated based on correct answers (1) or “don’t know”/incorrect responses (0). Mean scores for knowledge were derived by summing scores in each section and dividing by the number of items, then converted to percentages. A score of ≥ 60% (≥ 13 points) indicates adequate knowledge, while < 60% (< 13 points) indicates inadequate knowledge.
Tool 3: Women’s knowledge regarding most common drugs that cause congenital anomalies questionnaire sheet: Total global scores were derived from 6 questions (1 point each) based on correct answers (1 point) or “don’t know”/incorrect (0 points). Mean scores were calculated by summing scores, dividing by the number of items, and converting to percentages. A score of ≥ 60% (≥ 4 points) reflects adequate knowledge; < 60% (< 4 points) indicates inadequate knowledge.
Supportive material: The researcher created an educational booklet in simple Arabic to raise awareness among women about teratogenic medications during pregnancy. It includes instructions for drug intake, highlights common teratogenic drugs that may lead to congenital anomalies, such as Imodium causing cleft lip and palate, and provides basic knowledge of congenital anomalies and their effects on pregnant women’s health.
Fieldwork: The study involved four phases: assessment, planning, implementation, and evaluation. Data was collected through interviews with pregnant women, questionnaires, and interviews. An educational booklet was created based on the assessment data. Pregnant women participated in pretest questionnaires and sessions in Arabic. The evaluation phase measured knowledge, attitude & behavioral changes resulting from the educational program. Ethical approval was obtained from Beni-Suef University’s research ethics committee and Beba Hospital. Data was analyzed using descriptive statistics and chi-square test.
Results
Figure (1) reveals that 46.6% of women had previous births through cesarean section and 27.4% had normal vaginal birth.
Table (1) illustrates that there was a statistically significant improvement during the posttest among the studied pregnant women regarding congenital anomalies and the drug. Women were compared with the pretest, and it was noticed that 41.6%, 46.6%, and 43.3% of the studied pregnant women had correct knowledge regarding any medication that can be used at any stage of pregnancy, the name of the medicine that has been prescribed by the doctor, and the use of all the medicines that they were currently taking during the pretest, which was improved in the posttest to become 70.9%, 63.1%, and 67.3% of women, respectively. The same table reveals that 46.9% & 47.8% of the studied pregnant women had correct knowledge regarding congenital malformations, which are structural or functional challenges that can be identified inside the uterus before birth, and medications without consulting a doctor do not lead to congenital anomalies during the pretest, which improved in the posttest to become 66.2% & 74.6% of women, respectively.
Figure (2) shows that it was noticed that 86.3% of women had an inadequate knowledge level regarding congenital anomalies and the drug that causes them during the pretest; that regressed to only 17.0% posttest.
Table (2) presents that, there was a statistically significant improvement during posttest among the studied pregnant women regarding most common drugs that cause congenital anomalies comparing with pretest and noticed that, (38%, 45.3% & 45%) of the studied pregnant women had correct knowledge regarding taking Imodium tablets during pregnancy without consulting a doctor may lead to a cleft palate, taking anal Brill tablets to treat pressure during pregnancy without consulting a doctor may lead to fetal failure and taking clonazepam tablets in the first trimester during pregnancy without consulting a doctor may lead to phenomenon of neonatal withdrawal during pretest which improved posttest to become (89.9%, 86.9% & 71.8%) of women, respectively.
Figure (3) shows that it was noticed that 85.2% of women had an inadequate knowledge level regarding the most common drugs that cause congenital anomalies; that regressed to 21.8% posttest.
Table 1: Percentage distribution of the studied pregnant women’s knowledge regarding to congenital anomalies and the drug that causes (n=358).
| Congenital anomalies and the drug that causes women | Pretest | Posttest |
X2 |
p value |
||||||
| Correct | Incorrect | Correct | Incorrect | |||||||
| No. | % | No. | % | No. | % | No. | % | |||
| Any medication can be used at any stage of pregnancy. | 149 | 41.6 | 209 | 58.4 | 254 | 70.9 | 104 | 29.1 | 25.269 | 0.000** |
| Some medications may be more suitable to be used during pregnancy. |
117 |
32.7 |
241 |
67.3 |
267 |
74.6 |
91 |
25.4 |
31.653 |
0.000** |
| A non-prescribed medication can be used during pregnancy. | 112 | 31.3 | 246 | 68.7 | 289 | 80.7 | 69 | 19.3 | 17.769 | 0.000** |
| Wrong drug choice can affect the formation of the fetus and the health of mother. | 133 | 37.2 | 225 | 62.8 | 242 | 67.6 | 116 | 32.4 | 37.192 | 0.000** |
| The pharmacist should provide all necessary information and advice regarding the medication before using it. | 137 | 38.3 | 221 | 61.7 | 247 | 69.0 | 111 | 31.0 | 54.767 | 0.000** |
| It is safe to take common medications and over-the-counter drugs without the physician’s or pharmacist’s advice. | 129 | 36.0 | 229 | 64.0 | 286 | 79.9 | 72 | 20.1 | 6.077 | 0.014* |
| Some medications should never be used in pregnancy regardless of condition. | 110 | 30.7 | 248 | 69.3 | 261 | 72.9 | 97 | 27.1 | 28.754 | 0.000** |
| Taking a folic acid tablet before pregnancy and during the first three months contributes to preventing congenital malformations. |
130 |
36.3 |
228 |
63.7 |
221 |
61.7 |
137 |
38.3 |
76.766 |
0.000** |
| Know the name of the medicine that has been prescribed by the doctor. | 167 | 46.6 | 191 | 53.4 | 226 | 63.1 | 132 | 36.9 | 39.373 | 0.000** |
| know the use of all the medicines that are currently being taken | 155 | 43.3 | 203 | 56.7 | 241 | 67.3 | 117 | 32.7 | 45.484 | 0.000** |
| Know that medicines can also show adverse effects. | 130 | 36.3 | 228 | 63.7 | 246 | 68.7 | 112 | 31.3 | 46.183 | 0.000** |
| Know that all medicine that is taken might not be safe in pregnancy. | 146 | 40.8 | 212 | 59.2 | 259 | 72.3 | 99 | 27.7 | 46.545 | 0.000** |
| Know that unnecessary medicine taken by the pregnant mother can show adverse effects on the health of the mother and fetus. |
158 |
44.1 |
200 |
55.9 |
283 |
79.1 |
75 |
20.9 |
17.734 |
0.000** |
| Know that exposure to unnecessary medicine during preg- nancy can affect fetal organogenesis and development. | 151 | 42.2 | 207 | 57.8 | 260 | 72.6 | 98 | 27.4 | 39.955 | 0.000** |
| Congenital malformations are structural or functional chal-
lenges that can be identified inside the uterus before birth. |
168 | 46.9 | 190 | 53.1 | 237 | 66.2 | 121 | 33.8 | 100.522 | 0.000** |
| The side effect of the congenital anomalies is fetal growth retardation. | 166 | 46.4 | 192 | 53.6 | 260 | 72.6 | 98 | 27.4 | 87.891 | 0.000** |
| The kinship between the son may lead to congenital anomalies. | 145 | 40.5 | 213 | 59.5 | 257 | 71.8 | 101 | 28.2 | 44.576 | 0.000** |
| The fast food may lead to congenital anomalies. | 157 | 43.9 | 201 | 56.1 | 272 | 76.0 | 86 | 24.0 | 32.071 | 0.000** |
| Medications without consulting a doctor do not lead to congenital anomalies. | 171 | 47.8 | 187 | 52.2 | 267 | 74.6 | 91 | 25.4 | 54.815 | 0.000** |
| Obesity may lead to congenital malformation. | 162 | 45.3 | 196 | 54.7 | 265 | 74.0 | 93 | 26.0 | 36.892 | 0.000** |
| Radiation does not lead to congenital malformation. | 153 | 42.7 | 205 | 57.3 | 271 | 75.7 | 87 | 24.3 | 22.829 | 0.000** |
| Total (mean±SD) | 8.508±3.447 | 15.106±4.097 | 6.743 | 0.009** | ||||||
* Statistically significant at p≤0.05 ** High statistically significant at p≤0.01
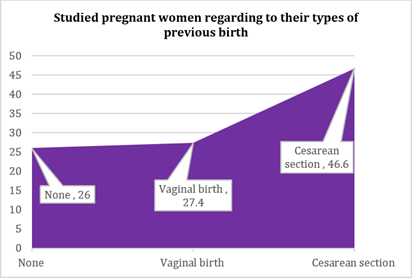 Figure 1: Percentage distribution of the studied pregnant women regarding to their types of previous birth.
Figure 1: Percentage distribution of the studied pregnant women regarding to their types of previous birth.
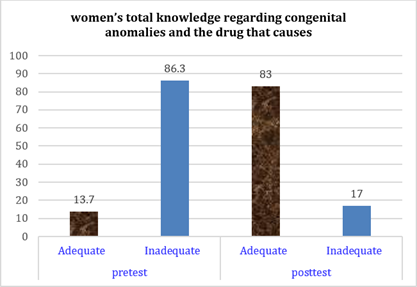 Figure 2: Women’s total knowledge regarding congenital anomalies and the drug that causes.
Figure 2: Women’s total knowledge regarding congenital anomalies and the drug that causes.
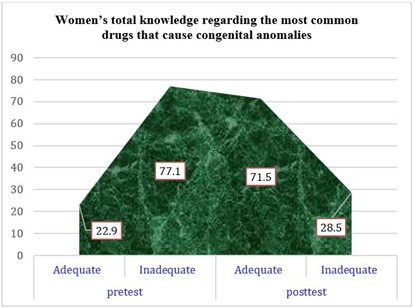 Figure 3: Women’s total knowledge regarding the most common drugs that cause congenital anomalies.
Figure 3: Women’s total knowledge regarding the most common drugs that cause congenital anomalies.
Table 2: Percentage distribution of the studied pregnant women’s knowledge regarding to most common drugs that cause congenital anomalies (n=358).
|
Most common drugs that cause congenital anomalies |
Pretest | Posttest |
X2 |
p value |
||||||
| Correct | Incorrect | Correct | Incorrect | |||||||
| No. | % | No. | % | No. | % | No. | % | |||
| Taking thalidomide during pregnancy without consulting a doctor may lead to hearing defects and lack of limb development. |
153 |
42.7 |
205 |
57.3 |
308 |
86.0 |
50 |
14.0 |
7.025 |
0.008** |
| Taking Imodium tablets during pregnancy without consulting a doctor may lead to a cleft palate? | 136 | 38.0 | 222 | 62.0 | 322 | 89.9 | 36 | 10.1 | 3.926 | 0.048* |
| Taking Analbrill tablets to treat pressure during pregnancy without consulting a doctor may lead to fetal failure? | 162 | 45.3 | 196 | 54.7 | 311 | 86.9 | 47 | 13.1 | 5.064 | 0.024* |
| Taking diazepam in the first trimester of pregnancy may
lead to shortness of breath and muscle relaxation in the fetus. |
159 |
44.4 |
199 |
55.6 |
269 |
75.1 |
89 |
24.9 |
12.041 |
0.001** |
| Taking methergine tablets will lead to fetal growth retardation, premature birth, and low fetal weight. | 151 | 42.2 | 207 | 57.8 | 271 | 75.7 | 87 | 24.3 | 9.071 | 0.003** |
| Taking sulfasalazine in the first trimester of pregnancy without consulting a doctor may lead to enlarged head size, ventricular septal defect, and cleft palate. |
143 |
39.9 |
215 |
60.1 |
278 |
77.7 |
80 |
22.3 |
6.734 |
0.009** |
| Taking rifaximin tablets during pregnancy without consult- ing a doctor may lead to partially open eyes, cleft palate, and short jaw in the fetus. |
148 |
41.3 |
210 |
58.7 |
254 |
70.9 |
104 |
29.1 |
12.790 |
0.000** |
| Taking corticosteroids in the first trimester during pregnan- cy without consulting a doctor may lead to low birth weight, the toxicosis stage, and cleft lip. |
128 |
35.8 |
230 |
64.2 |
262 |
73.2 |
96 |
26.8 |
5.952 |
0.015* |
| Taking temazepam in the first trimester during pregnancy without consulting a doctor may lead to neonatal withdrawal syndrome. |
151 |
42.2 |
207 |
57.8 |
270 |
75.4 |
88 |
24.6 |
11.907 |
0.001** |
| Taking clonazepam tablets in the first trimester during pregnancy without consulting a doctor may lead to the phenomenon of neonatal withdrawal. |
161 |
45.0 |
197 |
55.0 |
257 |
71.8 |
101 |
28.2 |
3.953 |
0.047* |
| Total (mean±SD) | 4.167±1.862 | 7.826±1.770 | 5.432 | 0.020* | ||||||
* Statistically significant at p≤0.05 ** High statistically significant at p≤0.01
Discussion
Self-medication is a serious health hazard that can lead to a variety of difficulties and considerable challenges for individuals and communities, particularly in pregnant women. Self-medication is a global issue that demands attention due to the possible risk not only to pregnant women but also to their unborn fetuses [25-29]. Medication use during pregnancy has been a concern both for the mother and fetus since the discovery of birth defects resulting from the thalidomide crisis in early pregnancy; this necessitates critical evaluation of the risk level of medication used during pregnancy [30]. That is why the current study was conducted to evaluate the effect of an educational program on enhancing pregnant women’s knowledge regarding teratogenic medications and the most common drugs that cause congenital anomalies.
Regarding types of previous births and place of birth, the current study demonstrated that less than half of pregnant women had cesarean sections. And more than one-third of them delivered at a public hospital. These findings were consistent with Almatrafi et al. (2024), who investigated “Awareness and Attitude of Women about the Teratogenic Effect of Drugs during Pregnancy” and found that the minority of the participants delivered at a public hospital via cesarean section [30]. This may be related to low socio-economic level and decreased awareness.
Overall, after the program, the pregnant women’s knowledge regarding teratogenic medications and the most common drugs that cause congenital anomalies was improved. Consequently, the implementation of the program improved the overall good knowledge grades of women. This improvement could be attributed to the implemented educational program and the lecture and positive reinforcement, as well as a wide variety of educational methods used [32-36]. Furthermore, the Arabic booklets that were distributed were essential for acquiring and remembering knowledge. Brief booklets that are written in plain language, have lots of eye-catching illustrations, and complement other teaching strategies are the best for their purposes. The NTL’s Pyramid of Learning, developed by Edgar Dale, demonstrated that people can retain 20.0% of what they see and hear (audiovisual) and 10.0% of what they read, according to Masters. According to the same author, a discussion can help one remember 50.0% of what they have learned [37-39].
Concerning knowledge of the studied pregnant women regarding to congenital anomalies and the drug that causes teratogenicity; the current study revealed that there was a statistical significant improvement during posttest among the studied pregnant women regarding congenital anomalies and the drug that causes them comparing with pretest and noticed that, less than half of the studied pregnant women had correct knowledge regarding any medication can be used at any stage of pregnancy, the name of the medicine that has been prescribed by the doctor and know the use of all the medicines that you are currently taking during pretest which was improved posttest to become more than two third of women.
These findings were consistent with Almatrafi et al. (2024), who investigated “Awareness and Attitude of Women about the Teratogenic Effect of Drugs during Pregnancy” and found that there was a statistically significant improvement in pregnant women’s knowledge regarding drug safety and teratogenic risks [30].
The study also reported that less than half of the studied pregnant women had correct knowledge regarding congenital malformations, which are structural or functional challenges that can be identified inside the uterus before birth, and medications without consulting a doctor do not lead to congenital anomalies during the pretest, which improved the posttest to become less than three-quarters of women.
This finding aligns with the cross sectional study by Alemu et al. (2023), who studied “Pregnant women’s knowledge of birth defects and associated factors in referral hospitals of the Amhara region” and reported that only about less than half of pregnant women had adequate knowledge about birth defects [40]. The observed improvement clearly demonstrates the effectiveness of structured educational interventions in correcting common misconceptions and increasing pregnant women’s awareness of the potential risks associated with unsupervised medication use during pregnancy.
Conclusion
The study also showed improvements in understanding common drugs that cause congenital anomalies, such as Imodium, Anabril, and clonazepam, which improved posttest. Additionally, the study found that pregnant women with correct knowledge of medication and congenital anomalies during pregnancy showed significant improvement posttest. Compared to the pretest.
Collaborate with public health organizations to implement national awareness programs focusing on educating pregnant women about teratogenic medications and offering resources for safer pregnancy practices.
Recommendations
Collaborate with public health organizations to implement national awareness programs focusing on educating pregnant women about teratogenic medications and offering resources for safer pregnancy practices.
References
- Teratogenic effect of isotretinoin in both fertile females and Experimental and Therapeutic Medicine, 21(5), 534.
- Kaleelullah, A., & Garugula, N. (2021). Teratogenic genesis in fetal malformations. Cureus, 13(2).
- Hassan H., Saber N., Sheha E. (2019). Comprehension of Dyspareunia and Related Anxiety among Northern Upper Egyptian women: Impact of Nursing Consultation Context Using PLISSIT Model. Nursing & Care Open Access Journal, 6(1): 1-19. DOI: 10.15406/ncoaj.2019.06.00177
- Malk R., Fahem E., Hassan H., Soultan A. (2022). Efficacy of Training Program on Nurses Performance regarding Preventive Measures of Venous Thromboembolism among Critical Pregnant Women. Egyptian Journal of Health Care, 13(2): 401-413. DOI: 10.21608/EJHC.2022.230390
- Hassan , Gamel W., Sheha E., Sayed M., Arafa A. (2019). Menstrual disorders Necessitating Counseling among Studentsin Beni-Suef University. Clinical Nursing Studies, 7(2): 29-36. doi:10.5430/cns.v7n2p29
- Eid S., Abou-Shabana K., Hassan A., Hassan H. (2023). Effect of Pre-Gynecological Examination Counseling Sessions on Relieving Women’s Pain, Discomfort and Enhancing their Satisfaction. Journal of Nursing Science - Benha University, 4(1): 751-768.
- Hassan H., Eid , Hassan A., Abou-Shabana K. (2022). Pre-Gynecological Examination: Impact Counseling on Women’s Pain, Discomfort, and Satisfaction. American Journal of Public Health Research, 10(2): 63-75
- Abou-Shabana K., Hassan A., Eid S., Hassan H. (2022). Effect of Counseling Sessions on Women’s Satisfaction during Gynecological Journal of Obstetrics Gynecology and Reproductive Sciences, 6(4): 1-10. DOI: 10.31579/2578- 8965/119
- Hassan , Gooda W., Ahmed T., Farag D. (2025). Marital, Sexual Satisfaction and Quality of Life among Post-hysterectomy Women: Impact of Nursing Counseling Guided by BETTER Model. Egyptian Journal of Health Care, 16 (1): 99-116. Doi: 10.21608/ejhc.2025.402051
- Fowler JR, Jenkins SM, Jack BW. Preconception Counseling. [Updated 2023 Jun 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441880/
- Farag & Hassan H. Maternal Postpartum Sleep disturbance and Fatigue: Factors Influencing. ARC Journal of Nursing and Healthcare, 2019; 5(2): 33-46. doi: http://dx.doi.org/10.20431/2455-4324.0502005
- Hassan H., Zahran K., Youness E., Nady F., (2015). Pregnant Women’s Awareness, Intention and Compliance regarding Folic Acid Usage for Prevention of Neural Tube Defects According to Health Belief Model in Beni-Suef Pyrex Journal of Nursing and Midwifery, 1(3): 13-26.
- Hassan H., Gooda W., Nashed N. Correlation between Women’s Knowledge, Life Style and Impact Level of Social Networking Sites on Women After Abortion Using Counseling Based On PLISSIT Model. American Journal of Public Health Research, 2025; 13(5):(2025): 199-207. doi: 10.12691/ajphr-13-5-1.
- Hassan , Abd-ELhakam F., Kasem E. (2025). Androgen-related Alopecia and Infertility: Impact of Lifestyle Modifications. International Journal of Clinical Research and Reports, 4(2): 1-6. DOI: https://doi.org/10.31579/2835-785X/071
- Hassan , Abd-ELhakam F., Ali E. (2025). Effect of Life Style Modification Implemented Program Among Infertile Women with Poly Cystic Ovary Syndrome on Obesity and Menstrual Regulation. Journal of Clinical and Laboratory Research, 8(2): 1-7. DOI:10.31579/2768-0487/166.
- Hassan , Abd-ELhakam F., Ali E. Effect of Life Style Modification Implemented Program Among Infertile Women with Poly Cystic Ovary Syndrome on Obesity and Menstrual Regulation. Journal of Clinical and Laboratory Research, 2025; 8(2): 1-7. DOI:10.31579/2768-0487/166
- Hassan , Abd-ELhakam F., Ali E. Infertility and Obesity: Impact of Lifestyle Modification. American Journal of Nursing Research, 2025; 13(3): 59-67. doi: 10.12691/ajnr-13-3-1.
- Nady , Zahran K., Youness E., Hassan H. (2014). Women’s Knowledge and Perception about Benefits of Folic Acid Intake Before and During Pregnancy According to Health Belief Model in Beni-Suef City. Assuit Scientific Nursing Journal, 2(3): 1-13.
- Hassan , Nady F., Youns E., Zahran K. (2016). Call for Change Level of Knowledge, Awareness and Attitude to Follow A High Folate Diet Among Pregnant Women. IOSR Journal of Nursing and Health Science, 5(1): 93-100. doi: 10.9790/1959- 051293100
- Sheha , Hassan H., Gamel W. Association between pre-pregnant overweight and obesity and periodontal disease during pregnancy: a cross sectional study. International Journal of Studies in Nursing. 2018; 3(1): 1-21. doi:10.20849/ijsn. v3i1.207.
- Kandhasamy, , Lepigeon, K., Baggio, S., Ce line, R., Ceulemans, M., Winterfeld, U., & Panchaud, A. (2025). Risk of adverse obstetrical and neonatal outcomes in women consuming recreational drugs during pregnancy. BMC pregnancy and childbirth, 25(1), 456.
- Dukare, S,G. Wagh,A, B & Waje, M,R. (2024). Understanding Teratogenicity In Pregnancy: A Comprehensive International Journal of Creative Research Thoughts. Volume 12, Issue 4 April 2024 | ISSN: 2320-2882
- Devkota, , Khan, G. M., Alam, K., Sapkota, B., & Devkota, D. (2017). Impacts of counseling on knowledge, attitude and practice of medication use during pregnancy. BMC pregnancy and childbirth, 17(1), 131.
- Elfeshawy,N. Zenhom,S & Elsayed,H. (2022). Assessment of Self-Medication Practices among Pregnant Women in Mansoura university hospital: Mansoura Nursing Journal (MNJ) 9. No. 2 – 2022 Print ISSN: 2735 – 4121 Online ISSN: 2735 – 413X
- Hassan , Badr Elden S., Hamdi S., Aboudonya M. (2021). Control Poly-Pharmacy: Elderly Patients’ Practices. American Journal of Pharmacological Sciences, 9(2): 56-62. doi: 10.12691/ajps-9-2-2.
- Hassan , Badr-Elden S., Hamdi S., Aboudonya M. (2021). Control Poly-Pharmacy: Elderly Patients’ Perception. American Journal of Medical Sciences and Medicine, 9(3): 82-88. doi: 10.12691/ajmsm-9-3-4.
- Aboudonya , Badr Elden S., Hassan H., Hafez S. (2022). Knowledge And Practices Used By Old Age Patients To Control Polypharmacy. Nile journal for geriatric and gerontology, 5(1): 80-91. DOI: 10.21608/NILES.2022.197281.
- Hassan , Badr Elden S., Hamdi S., Aboudonya M. (2021). Poly- Pharmacy among Elderly Patients: Perception and Practices. Journal of Nursing and Community Medicine, 1(1): 1-6.
- Ibironke C. Ojo,etal. (2020). Factors Influencing Self-Medication Practice among Pregnant Women Attending Antenatal Clinic in Primary Health Facilities in Akure South Local Government, Ondo State.” IOSR Journal of Nursing and Health Science, 9(2), 16-22
- Almatrafi, M. S., Alsuwailem, H. S. A., Alanazi, W. H. A., Alshammari, S. M. A., Alanazi, F. S. R., Alanazi, W. K. M., ... & Fawzy, S. (2024). Awareness and Attitude of Women about The Teratogenic Effect of Drugs During Pregnancy: A Pilot Study. Bahrain Medical Bulletin, 46(4).
- Hassan H. (2019): Integrative Nursing Science in Women’s Pre-conceptional Wellness. International Journal of Health and Biological Sciences; 2(1): 17-18.
- Hassan , Mohamady Sh., & Abd El-Gawad N. (2017): Protocol for improving nursing performance towards placentalexamination at labor units. Clinical Nursing Studies; 5(2): 1-11. http://dx.doi.org/10.5430/cns.v5n2p1.
- Gamel W., Genedy A., Hassan H. Impact of Puerperal Sepsis Self-Care Nursing Guideline on Women’s Knowledge and American Journal of Nursing Research, 2020; 8(2): 132-141. doi:10.12691/ajnr-8-2-1
- Hassan H., Abd-ELhakam F., Kasem E. (2025). Relationship between Infertile Overweight and Polycystic Ovary Syndrome Women’s Characteristics and Lifestyle Habits: An Interventional Journal of General medicine and Clinical Practice, 8(8): 1-7. DOI:10.31579/2639-4162/285
- Nady , Said M., Youness E., Hassan H. Impact of Tailored Educational Program of Quality of Life Improvement on Women Undergoing Breast Cancer Treatment at El-Minia Region, Egypt. American Research Journal of Gynaecology. 2017; 1(1): 1-17. doi:10.21694/2577-5928.17001
- Masters (2013): Edgar Dale’s Pyramid of Learning in medical education: A literature review, Medical Teacher; 35(11): e1584-e1593. https://doi.org/10.3109/0142159X.2013.800636
- Hassan , Gooda W., Nashed N. (2025). Post Abortion Women’s Life Style: Impact of Counseling Based on PLISSIT Model. American Journal of Nursing Research, 13 (4): 89-96. doi: 10.12691/ajnr-13-4-1
- Abd-Elfattah , Mohamed A., Hassan H. (2025). Study women’s attitude regarding Oocyte Cryopreservation: The Impact of an Educational Initiative. American Journal of Public Health Research, 13(5)
- Nashed N., Hassan H., Gooda W. (2025). Impact of Post Abortion Counseling Based on PLISSIT Model on Women’s Life Egyptian Journal of Health Care, 16 (2): 1009-1028. Doi: 10.21608/ejhc.2025.438157.
- Alemu, F. , Desta, A. A., & Fetene, D. (2023). Pregnant women’s knowledge of birth defects and associated factors in referral hospitals of Amhara region.
This article licensed under the Creative Commons Attribution 4.0 International License CC-BY 4.0., which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are properly credited.