NL Journal of Dentistry and Oral Sciences
(ISSN: 3049-1053)
Bone Regeneration with Dentin: Histological Evaluation and Results of a Study on Implant Stability Expressed in ISQ
Author(s) : Miguel Ricardo Quevedo Bisonni, Javier Barbi Actis, Fernando Munoz Guzon, Jose Maria Suarez Quintanilla. DOI : 10.71168/NDO.01.01.106
Abstract
The aim of this article is to analyze bone regeneration using semi-demineralized autologous dentin as graft material in patients requiring alveolar preservation after dental extraction. Previous studies have demonstrated that dentin, due to its similarity to bone, can be an effective biomaterial for bone regeneration. The study was conducted on 11 patients, whose alveoli were preserved using semi-demineralized dentin, followed by implant placement after 6 months. Implant stability was assessed with the Ostell device, using ISQ values. The results revealed a significant increase in bone density after 6 months of regeneration and adequate implant stability (70 ISQ). Histological evaluations confirmed the formation of new bone tissue and the progressive resorption of the semi-demineralized dentin graft. Keywords: Bone regeneration, Autologous dentin, Alveolar preservation, ISQ, Ostell, Tooth Transformer
Introduction
With the introduction of the concept of prosthetically guided implantology, merely achieving osseointegration is no longer sufficient to consider a treatment successful. The correct placement of the implant should replicate the natural position of the extracted tooth’s root within its alveolus. However, in most cases, the alveoli have undergone a bone resorption process, requiring the selection of an alternative location. This deviation compromises not only masticatory function but also other key factors, such as the three-dimensional orientation of the implant, the esthetics of the emergence profile, and the presence of cantilevers [1]. These situations often necessitate the design of more complex prostheses, which may result in a lack of structural passivity, leading to adverse outcomes such as prosthetic fractures or peri-implant bone resorption. Moreover, deviating from the alveolar bone increases the risk of inadvertently invading sensitive anatomical structures, such as the maxillary sinus, the inferior alveolar canal, or the nasal cavities, adding complexity and risk to the procedure.
The decision-making process must be based on a logical approach tailored to the patient’s specific conditions, which is an essential requirement for the success of any implant rehabilitation. The diagnosis and treatment plan will largely depend on the morphological and structural characteristics of the alveolus prior to the extraction. In this analysis, not only is a detailed clinical inspection crucial, but also the diagnostic support provided by radiological images. Conventional 2D radiographs, along with the three-dimensional images generated by cone- beam computed tomography (CBCT), offer a more precise and comprehensive view, facilitating surgical and prosthetic planning and optimizing outcomes [2,3].
After a dental extraction, the alveolus undergoes a series of morphological, histological, and dimensional changes that affect both the bone structure and the surrounding soft tissues. Since the late 20th century, many authors have observed that bone reduction occurs both horizontally and vertically. Recent studies have shown that horizontal bone loss reaches up to 63%, which is greater than the vertical loss, typically ranging between 11-22% within the first 6 months post-surgery. Further gradual reduction occurs over the following 6 months [4].
Several authors agree in recommending the implementation of guided bone regeneration (GBR) techniques in cases where it is not feasible to place the implant in an ideal prosthetic position. This recommendation is particularly relevant in the anterior region, where managing the emergence profile becomes more complex due to high aesthetic and functional demands, as well as the need to preserve gingival harmony and integration with adjacent structures [5].
Numerous biomaterials are available for guided bone regeneration, each with intrinsic properties that influence their effectiveness in different ways. Regardless of their origin - whether synthetic (alloplastic), animal-derived (xenogeneic), obtained from human tissue banks (homologous), or from the patient themselves (autologous)- they all share one essential property: osteoconduction. This refers to their ability to provide a suitable matrix for the key processes involved in bone tissue regeneration [6].
However, only one of these materials exhibits two additional characteristics that make it unique: the presence of proteins that induce bone regeneration (osteoinduction) and the direct contribution of osteoblasts (osteogenesis). This material is autologous bone, which is considered the gold standard among biomaterials.
Despite its numerous advantages, autologous bone presents significant challenges, such as the limited availability of material, morbidity associated with the donor site, prolonged surgical intervention time, and a range of postoperative discomforts and complications. These include not only physical complications but also psychological effects that may negatively impact recovery [7,8]. These limitations have led the scientific community to seek more viable alternatives, and one of the biomaterials that has recently gained attention in certain research circles is autologous dentin.
Dentin as a Biomaterial for Autologous Regeneration
When a tooth is transplanted or reimplanted, repair processes are triggered in the affected area that culminate in ankylosis, that is, the integration of the tooth with the surrounding bone. Since the composition of cementum and dentin is similar to that of bone, osteoblasts deposit new material directly onto these structures, creating an ankylosed dentin-bone interface. This phenomenon is the same as that which occurs when avulsed teeth are successfully reimplanted. These findings led several scientists to suggest that both cementum and dentin, when properly treated, could be useful as graft materials [9,10].
Among the tissues that make up the tooth, dentin, after enamel, has the highest mineral content, even surpassing any bone derivative. However, it is not just this characteristic that contributes to its capacity for bone regeneration; its organic matrix also makes it comparable to autogenous bone (Fig. 1). This combination allows it to act as a suitable physical matrix on which new bone formations can be deposited, while also inducing osteoformation. Therefore, dentin can be considered an optimal biological and bioactive material for hard tissue regeneration.
Hard dental tissues originate from different embryonic layers: enamel is produced by ameloblasts of ectodermal origin, while dentin is formed by odontoblasts of mesodermal origin. Dentin, pulp, cementum, and alveolar bone share the same embryonic origin, as well as the composition of type I collagen and several proteins common among these tissues [11-13] (Fig. 2).
In 1967, Urist was a pioneer in using dentin and obtained positive results in animal studies. Over the past 55 years, numerous research teams have successfully explored the use of dentin as a promising biomaterial, highlighting its favorable properties for bone regeneration.
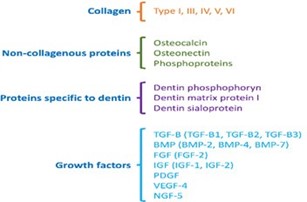
Fig.1 – Composition of the organic matrix of dentin
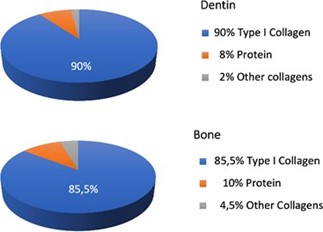
Fig.2 Comparison of bone and dentin matrices
Materials and Methods
This study was conducted at the Oral Surgery Teaching Unit of the Faculty of Medicine and Dentistry at the University of Santiago de Compostela. Based on previously published studies on this technique, we selected 11 patients who required dental extractions and subsequent alveolar preservation through regeneration with semi- demineralized autologous dentin grafts. Implants were placed in these patients six months after the regeneration procedure.
In addition to standard surgical instruments, two specific devices were used for this procedure. The first device is the Tooth Transformer (Fig. 3) (TT Tooth Transformer srl, Milan, Italy), a medical device designed to obtain demineralized dentin through two distinct cycles. In the first cycle, lasting up to 4 minutes, the tooth is ground into particles between 0.4 and 0.8 mm in size. In the second cycle, which lasts 25 minutes, the particles are demineralized, disinfected, and hydrated using liquids contained in single-use cartridges, resulting in demineralized dentin suitable for use as graft material in alveolar preservation techniques.
The second device used is the Ostell (Fig. 3) (W&H – Bürmoos, Austria), which uses resonance frequency (kHz) to measure the ISQ (Implant Stability Quotient), indicating implant stability: ISQ values below 60 suggest low stability, values between 60 and 65 indicate medium stability, and values above 70 are considered to indicate high stability.
Fig. 3 – Ostell and Tooth Transformer devices

Osstell Device

Tooth Transformer Device
The extracted teeth were processed immediately. After removing tartar, attached periodontal tissue, remnants of amalgams, composites, and other restorative materials, the teeth were sectioned into fragments measuring 4 to 5 mm. These fragments were placed in the Tooth Transformer device for 5 minutes, producing particles between 0.4 and 0.8 mm. A second cycle was then initiated in the device to demineralize, disinfect, wash, and hydrate the particles, thereby creating a biomaterial suitable for use.
The alveolus was filled with this material for preservation, covered with a collagen membrane, and then sutured using 4.0 Nylon sutures.
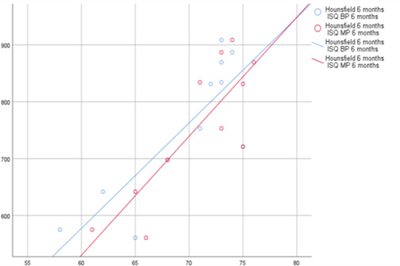
Three months after the surgery, the density of the regenerated alveolus was evaluated using Hounsfield Units and compared with a second evaluation conducted six months after the regeneration surgery and prior to implant placement surgery.
Results
At 3 months post bone regeneration, CBCT images showed that the average Hounsfield unit (HU) value was 583.64, with higher values in the lower anterior region compared to other areas of the mouth. In the second evaluation at 6 months, prior to implant placement, this value increased to 722.36, remaining higher in the lower anterior region. These values correspond to D3-type bone according to the Misch classification, although in the lower anterior region, the values approach the threshold for D2-type bone (850 Hounsfield units). At 6 months, the average bone density was observed to increase.
After implant placement, the stability of each implant was measured using the Ostell device, with an average ISQ value of 70, which is the minimum required for immediate loading of an implant. These measurements correlate with the good density achieved through the semi-demineralized dentin graft and the high implant stability in terms of ISQ. (Fig. 4)
Fig. 4
Additionally, histological samples from other patients were taken to evaluate the state of the regenerated tissue at 3, 6, and 8 months post-regeneration, and we observed the following:
In histological samples obtained at our teaching unit, three months after alveolar preservation using an identical technique, we observed the formation of new bone tissue around dentin particles, which exhibited partial resorption (Fig. 5). Our research team recently published results on the use of Tooth Transformer® technology applied after the extraction of supernumerary teeth, including canines and third molars. Although these studies were exclusively clinical, we were able to radiographically confirm adequate bone formation at 6 and 12 months post-surgery [12].
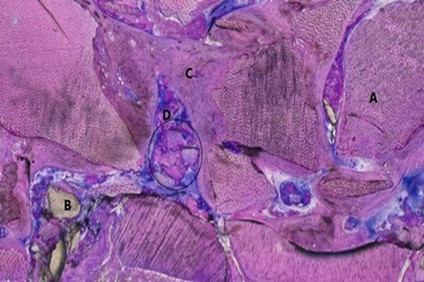
Fig.5 – Histological section 3 months: (A) Stained Dentin particles (B) Unstained Dentin particles (C) Developed bone tissue (D) Newly formed bone tissue around the dentin particles
Histological samples taken by our team revealed that, at six months, a significant portion of the dentin had been resorbed, though not as much as at eight months, when very few dentin particles were observed in the samples (Fig. 6).
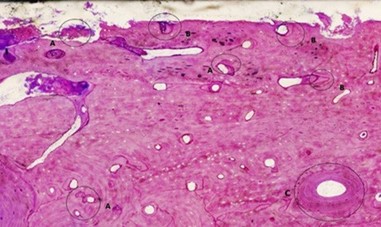
Fig.6 – Histological section 8 months: (A) Mature bone, with some dentin particles in the process of resorption. (B) Areas where these particles have notably integrated. (C) Formed bone tissue, with complete replacement of dentin particles by bone with varying degrees of trabeculation, presenting areas of bone remodeling, with the formation of lamellae around blood vessels.
Discussion
Currently, two distinct protocols have been developed for the use of demineralized dentin grafts as a bone substitute. The first involves a rigorous demineralization process, ensuring the graft is properly prepared. In contrast, the second protocol uses fresh autogenous dentin without the need for demineralization, directly leveraging its natural biological properties to promote bone regeneration.
As previously mentioned, dentin is a tissue with a higher degree of mineralization compared to bone, and its organic portion presents a remarkably similar composition. It not only shares a comparable proportion of type I collagen but also contains essential growth factors for bone regeneration, positioning it as a biomaterial with great osteoinductive potential. This second alternative, using the Tooth Transformer, the protocol we have been employing in our Oral Surgery Clinical Unit at the University of Santiago for the past six years - provides us with a dentin preparation that is completely free of bacteria. This ensures not only predictable structuring but also its immediate use as a biomaterial, offering a safe and efficient option for bone regeneration [14].
The studies conducted by Kim et al. in 2010, in which serial extractions of several permanent teeth were performed, followed by grinding and simultaneous use as graft material during implant placement [11], were crucial for initiating clinical trials in patients. Three months later, coinciding with the second surgical phase, small biopsies were taken, demonstrating that a significant portion of the dentin had been resorbed and replaced by new bone in percentages ranging from 39% to 79%.
Kabir’s research group was the first to systematically use demineralized dentin grafts following the extraction of an upper third molar, with the aim of preventing distal bone resorption of the second molar, a phenomenon that often occurs after this surgical procedure[13]. Through clinical and radiographic evaluations conducted at 3 and 12 months post-extraction, they confirmed that a significant portion of the demineralized dentin matrix was adequately replaced by new bone tissue, partially mitigating the undesirable effects on the second molar.
Conclusion
Since there is no osseointegration between the graft surface and the implant, it is desirable that the biomaterials used are progressively resorbable once they have fulfilled their function, thus allowing the formation of high- quality bone. Ideally, these biomaterials should be fully resorbable, with a gradual resorption process synchronized with the timing of bone regeneration. However, not all biomaterials possess this property, and some may remain at the regeneration zone indefinitely.
In the case of semi-demineralized dentin grafts, we have observed that resorption is gradual and nearly complete, from the beginning of the regenerative process until 8 or 9 months. Additionally, we have confirmed that the regenerated zone, at 6 months, presents an optimal bone density for implant insertion, and that the implants, once placed, show a very suitable ISQ stability index for immediate loading. Moreover, at 9 months (three months after implant placement), the presence of dentin is virtually nonexistent, ensuring full contact at the bone-implant interface.
For all the reasons mentioned, we consider that semi-demineralized dentin grafts should be the material of choice (whenever possible) in cases of alveolar preservation. However, we acknowledge that further studies are still required to confirm this with absolute certainty.
References
1. Misch CE. Implantologí�a contemporánea. 3ª ed. Barcelona: Elsevier España; 2009.
2. Elian N, Cho S, Froum S, Smith RB, Tarnow DP. A simplified socket classification and repair technique. Pract Proced Aesthet Dent. 2007;19(2):99-104.
3. Chu S, Sarnachiaro G, Hochman M, Tarnow D. Subclassification and clinical management of extraction sockets with labial dentoalveolar dehiscence defects. Compend Contin Educ Dent. 2015;36(7):516-522.
4. Rebolledo Cobos M, Harris Ricardo J, Higgins Samper E, Molinares Camargo L. Cicatrización y regeneración ósea de los maxilares después de una quistectomí�a: reporte de un caso y revisión de la literatura. Univ Odontol. 2011;30(65):71-78.
5. Caubet Biayna J, Heras Rincón I, Sánchez Mayoral J, Morey Mas M, Iriarte Ortabe J I. Manejo de defectos óseos anteroposteriores en el frente estético. Rev Esp Cirug Oral y Maxilofac. 2009; 31(2):81-97
6. Barone A, Nannmark U. Bone, Biomaterials & Beyond – Técnicas quirúrgicas y biomateriales para el aumento de los tejidos duros y blandos en cirugí�a implantar. AMOLCA, Actualidades Médicas, C.A;2015
7. Kim YK, Kim SG, Byeon JH. Development of a novel bone grafting material using autogenous teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod; 2010; 109:496.
8. Calvo Guirado J, Fernández M. Utilización de dentina como biomaterial para relleno óseo. El dentista moderno. 2019;38 43.
9. Binderman, I., Hallel, G., Nardy, C., Yaffe, A., & Sapoznikov, L. Processing extracted teeth for immediate grafting of autogenous dentin. Implant Pract US. 2015;8(2):43-46.
10. Minetti E, Gianfreda F, Palermo A, Bollero P. Autogenous Dentin Particulate Graft for Alveolar Ridge Augmentation with and without Use of Collagen Membrane: Preliminary Histological Analysis on Humans. Materials. 2022;15(12):4319.
11. Kim YK, Kim SG, Byeon JH, Lee HJ, Um IU, Lim SC, et al. Development of a novel bone grafting material using autogenous teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 109 (4): 496-503
12. Quevedo Bisonni M, Sciaini Lewis V, Rodrí�guez Pena K, Núñez Otero M, Barbi Actis J, Tábara Rodrí�guez JJ. Utilización de la tecnologí�a Tooth Transformer y los dientes incluidos del paciente, como material de injerto en un tratamiento multidisciplinar. RCOE. 2022;27(4):284-292.
13. Kabir AM, Murata M, Kusano K, Akazawa T, Shibata T. Autogenous demineralized dentin graft for third molar socket regeneration. Dentistry. 2015;5(11):11-14. en un tratamiento multidisciplinar. RCOE. 2022;27(4):284-292.
14. Guirado, J. L. C. (2017). Nuevo procedimiento para procesar los dientes extraí�dos como injerto en alveolos postextracción. Gaceta Dent.2019;(290):96-113.
This article licensed under the Creative Commons Attribution 4.0 International License CC-BY 4.0., which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are properly credited.