NL Journal of Dentistry and Oral Sciences
(ISSN: 3049-1053)
Immediate Guided Implantation with Aesthetic Loading: A Case Report
Author(s) : Faten Khanfir, Mohamed Ali Hedhli, Mohamed Tlili, Mohamed Salah Khalfi, Faten Ben Amor. DOI : 10.71168/NDO.02.05.130
Abstract
Background: Immediate implant placement with aesthetic loading in the anterior maxilla is a highly demanding procedure that requires precision, atraumatic extraction, and optimal planning. The use of a digital surgical guide has improved the predictability of this protocol, offering enhanced accuracy, reduced morbidity, and improved patient satisfaction. Case Presentation: We report the case of a 54-year-old female patient who presented with an irrecoverable maxillary left lateral incisor. Following CBCT analysis and intraoral scanning, a tooth-supported surgical guide was designed using 3Shape TRIOS software. Atraumatic extraction was performed, and a 3.6 × 12 mm Biotech implant was placed immediately with the aid of the surgical guide. The implant achieved primary stability (>35 Ncm), allowing for immediate aesthetic provisionalization with a PMMA crown. After three months of successful osseointegration, a definitive zirconia crown was fabricated and cemented. Results: The patient demonstrated uneventful healing, satisfactory osseointegration, and stable soft tissues. Both functional and aesthetic outcomes were favorable, with high patient satisfaction. Conclusion: Immediate implant placement with guided surgery and aesthetic loading represents a predictable treatment option in selected cases, providing functional rehabilitation and optimal aesthetic integration. This approach highlights the importance of careful case selection, precise digital planning, and adherence to surgical protocols to minimize complications and ensure clinical success. Keywords: Immediate implant placement, Guided surgery, Aesthetic loading, CBCT, Digital dentistry.
Introduction
Implant-supported rehabilitation in the anterior sector represents one of the most delicate challenges in our field, requiring particular expertise.
Aesthetic restoration and immediate implant extraction involves atraumatic extraction, followed by implant placement, and finally the creation of a temporary crown. This protocol offers significant advantages for both patient and practitioner, including psychological satisfaction, time savings and soft tissue management for optimal esthetic integration.
This protocol requires perfect knowledge of the anatomical structures visible on the different CBCT sections, which becomes more precise with the use of a digital surgical guide enabling the dentist to place the implant in the position of the future prosthesis already planned in advance.
Through a clinical case study, we highlight the importance of using a digital surgical guide for immediate implant placement. This case study highlights the many advantages inherent in this procedure, underlining its positive impact on clinical results.
Observation
A 54-year-old female patient in good general health visited the outpatient department of the University Hospital Clinic of Odontology in Monastir, Tunisia, for therapeutic management of her left maxillary lateral incisor.
Endo-buccal examination (Figure 1) revealed the presence of the 22 roots.
Radiological examination (Figure 2) showed no periapical infection or desmodontal enlargement, and the presence of a thin layer of vestibular bone, so tooth 22 was deemed irrecoverable.
After discussing the treatment options with the patient, she opted for immediate implant-guided extraction with esthetic loading.
 Figure 1: Occlusal view of the maxilla showing the fractured crown of 22.
Figure 1: Occlusal view of the maxilla showing the fractured crown of 22.
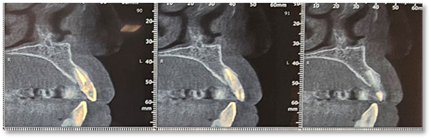 Figure 2: Sagittal sections of the CBCT of the patient.
Figure 2: Sagittal sections of the CBCT of the patient.
Operating Protocol
After scaling and root planning with hygiene motivation, we took a bimaxillary digital impression of the patient and planned a tooth-supported surgical guide based on the complementarity between the STL file from the digital impression and the DICOM file from the CBCT using the 3Shape TRIOS 3 software (Figure 3).
 Figure 3: Virtual planning for the tooth-supported surgical guide.
Figure 3: Virtual planning for the tooth-supported surgical guide.
Surgical Phase
The patient returned for her third appointment, corresponding to the surgical phase of treatment. After disinfecting the incisive-canine area, local anesthesia was administered. The maxillary left lateral incisor (tooth 22) was then atraumatically extracted to preserve the vestibular bone. (Figure 4) Following extraction, the surgical guide was positioned and stabilized, and the drilling sequence was initiated for the placement of a 3.6 mm × 12 mm Biotech implant (Figure 5).
 Figure 4: Atraumatic extraction of the 22.
Figure 4: Atraumatic extraction of the 22.
 Figure 5: Implant Placement.
Figure 5: Implant Placement.
After implant placement (Figure 5), the primary stability of the implant was satisfactory (greater than 35N), the provisional abutment was fixed (Figure 6) and a post-operative retroalveolar radiograph was taken for radiological control of the implant and adaptation of the provisional abutment (Figure 7) and finally PMMA resin was placed around the provisional abutment, and the occlusion was checked to ensure that the provisional prosthesis was underbite (Figure 8).
 Figure 6: Fixing the temporary abutment to the implant.
Figure 6: Fixing the temporary abutment to the implant.
 Figure 7: Post operative radiograph.
Figure 7: Post operative radiograph.
 Figure 8: Screwing of the provisional prosthesis.
Figure 8: Screwing of the provisional prosthesis.
Prosthetic Phase
After the 3-month period required for osseointegration of the implant, the patient was seen for a digital impression for the definitive prosthesis and the fabrication of a Ti-base zirconia abutment (Figure 9), noting that the patient was under monthly clinical and radiological control. The crown was sealed, and the patient is satisfied with her crown both aesthetically and functionally (Figure 10).
 Figure 9: Occlusal view of Ti-base zirconia abutment.
Figure 9: Occlusal view of Ti-base zirconia abutment.
 Figure 10: Final result of implant rehabilitation.
Figure 10: Final result of implant rehabilitation.
Discussion
Our clinical case represents an ideal example of immediate implant placement due to the presence of key indications for this technique, summarized as follows:
- Intact Vestibular Bone Wall: Pre- and post-extraction probing of the alveolar crest ensures identification of the vestibular cortical bone’s position, which is critical for determining the apico-coronal placement of the implant. A minimum thickness of 1mm is required for successful outcomes [2].
- Favorable Mucogingival Environment: This includes the absence of asymmetries, perforations, or very thin tissues, which helps prevent infection risks and aesthetic complications. A minimum of 2mm keratinized gingiva is recommended [2].
- Favorable Tooth and Residual Socket Anatomy: A minimum of three residual walls is necessary for success, as fewer than three walls increases the risk of Moreover, an ectopic tooth position or a misalignment between the extraction and implant sites may render immediate replacement impossible [3].
- Sufficient Bone Volume: Adequate bone volume must be evaluated to ensure successful treatment. The integrity of the vestibular bone plate, the bone height beyond the tooth roots, and the presence of bone septa between adjacent teeth are critical for success [1].
- Absence of Acute Infection and Suppuration: According to literature, active infection and suppuration are considered contraindications for immediate implant placement [4].
The guided immediate extraction-implantation method offers several benefits. It allows for a single, streamlined procedure without the need for a waiting period post-extraction, thereby eliminating multiple interventions and providing comfort during and after the operation, while also reducing stress and post-operative complications [5]. It also minimizes manipulation of the soft tissues and limits hard tissue resorption, a process that typically results in the loss of 40% of height and 60% of alveolar width within the first six months. This bone loss is exacerbated when the socket is damaged, such as by infection or the absence of a bone wall. This approach helps maintain adequate bone volume, which can be difficult to achieve after the usual healing period [6].
Additionally, extraction promotes a significant vascular supply due to the periodontal ligament and the opening of medullary spaces, which aids in the healing process [7,8].
However, it is important to note that the application of this method is limited, and failure rates are higher when protocols are not strictly followed. Among the disadvantages are the high cost, the risk of aesthetic complications, and the uncertainty in outcomes due to potential trauma to the socket during extraction [3,9].
This technique requires precision in execution, and while it offers significant benefits, there is a margin of error. The accuracy of the 3D-printed surgical guide may vary between 0.25mm and 0.5mm, and the cone beam CT scan carries an error margin of around 0.6mm, giving a total error margin between 0.85mm and 1.1mm [10,11].
Conclusion
Today, it is crucial to consider implantology from both an esthetic and a functional perspective. Patient expectations are evolving, as are techniques. What makes this approach particularly attractive is that the patient benefits from a new fixed tooth, offering an aesthetic result superior to that of a temporary removable prosthesis [12].
Thanks to advances in artificial intelligence and the use of a surgical guide, we are now able to treat complex cases, providing patients with less stressful and more comfortable care. However, clinical success depends on careful case selection. Immediate implant placement and esthetic loading should be reserved for specific patient profiles. The practitioner must assess the complexity of the case according to his or her experience, considering both early and delayed implant placement, without ruling out any possibility [9,12].
References
1. Siegenthaler DW, Jung RE, Holderegger C, Roos M, Hammerle CHF. Replacement of teeth exhibiting periapical pathology by immediate implants. A prospective, controlled clinical trial. Clin Oral Impl Res. 2007;18; 727–737.
2. Guillaume Leroux. Extraction, implantation et mise en esthetique immediate dans le secteur anterieur du maxillaire superieur. Medecine humaine et pathologie. 2016. ffdumas-01400884f
3. DR. YVES LAUVERJAT ET LAURENT BORDES LE 9 AOUT 2010 Interet clinique de l’extraction-implantation immediate https://www.lefildentaire.com/articles/clinique/implantologie
4. Dr. Thierry rouach le 21 fevrier 2011 donnees fondamentales de l’extraction-implantation immediate https://www.lefildentaire.com/articles/pratique/step-by-step
5. Nardy Casap, Chassiel Zeltser, Alon Wexler, Eyal Tarazi, and Rephael Zeltser. Immediate Placement of Dental Implants Into Debrided Infected Dentoalveolar Sockets. J Oral Maxillofac Surg 2007; 65: 384-392
6. Sclar AG. Guidelines for flapless surgery. J Oral Maxillofac Surg 2007: 65 (Suppl. 1): 20–32
7. Garber DA, Salama MA, Salama H. Immediate total tooth replacement. Compend Contin Educ Dent 2001: 22: 210–218.
8. Tarnow DP, Chu SJ, Salama MA, Stappert CF, Salama H, Garber DA, Sarnachiaro GO, Sarnachiaro E, Gotta SL, Saito H. Flapless postextraction socket implant placement in the esthetic zone: part 1. The effect of bone grafting and/or provisional restoration on facial-palatal ridge dimensional change – a retrospective cohort study. Int J Periodontics Restorative Dent 2014: 3: 323–331.
9. Extraction Implantation et Mise en Esthetique Immediates des Implants Unitaires Anterieurs https://www.ifcia-antoun.com/fr/publications/cas-cliniques/0153-Extraction-Implantation-et-Mise-en-Esthetique- Immediates-des-Implants Unitaires-Anterieurs via @IFCIA_Paris
10. Lin GH, Chan HL, Bashutski JD, Oh TJ, Wang HL. The effect of flapless surgery on implant survival and marginal bone level:a systematic review and meta-analysis. J Periodontol 2014: 8: 91–103. 13- Raes F, Cosyn J, Crommelinck E, Coessens P, De Bruyn H. Immediate and conventional single implant treatment in the anterior maxilla: 1-year results of a case series on hard and soft tissue response and aesthetics. J Clin Periodontol 2011: 38: 385–394
11. Kan JYK, Rungcharassaeng K, Deflorian M, Weinstein T, Wang HL, Testori T. Immediate implant placement and provisionalization of maxillary anterior single implants. Periodontol 2000. 2018;77:197-212.
12. S. Mate et al. Cas clinique et revue de litterature Facteurs decisionnels d’une extraction implantation mise encosmetique immediate unitaire Med Buccale Chir Buccale 2015;21:219-224
This article licensed under the Creative Commons Attribution 4.0 International License CC-BY 4.0., which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are properly credited.